CARE IN MOTION with The Invisible Disabilities Association® and TINNITUS: Symptoms, Diagnosis, Treatment and Outcomes
Ringing in the ears can occur after traumatic brain injury, COVID, vaccine, or exposure to loud noise. While treatment options are limited, there are novel options geared to improve Quality of Life
The Invisible Disabilities Association® is here to listen to you, believe in you, and to support you through 2023 and beyond.
Join in for a Great 2023 and Do Something New! Won’t You Join Me and Follow IDA today on Facebook, Twitter, and LinkedIn
The Invisible Disabilities Association® (IDA)
Do you have an invisible disability, or know someone who does? If you are ill with something that does not yet have a formal diagnosis, and you know it, you can help describe it to others. But perhaps more importantly, you can KNOW WHAT IT IS and that there are others who support you and your diagnosis as being “invisible”.
If you don’t know if you have an invisible disability, read on because this can be a life-changing awareness. Because if you want a different outcome, you need to make changes. Said another way, when you make changes, you change outcome (and maybe you’ll feel better, get more support, and have more hope)!
If you have an invisible disability, you can wear a lanyard ID to show you need help at an airport or while traveling:
Order an Invisible Disabilities® ID CARD: https://bit.ly/3GHBo9B from IDA®.
What is an Invisible Disability?
As Vice Chair of IDA and for background information, please allow me to provide you with a portion of our website definition:
In general, the term disability is often used to describe an ongoing physical or mental challenge. This challenge could be a well-managed bump in life or a mountain that creates severe changes and loss. Either way, this term should not be used to describe a person as weaker or lesser than anyone else! Every person has a purpose, uniqueness, and value, no matter what hurdles they may face. When we define invisible disability, it helps us understand the subtle differences and challenges each person experiences in their daily lives.
Also, just because a person has a disability, does not mean they are disabled.
Many living with these challenges are still fully active in their work, families, sports or hobbies. Some with disabilities can work full or part-time, but struggle to get through their day, with little or no energy for other things. Others are unable to maintain gainful or substantial employment due to their disability, have trouble with daily living activities and need assistance with their care.
According to the Americans with Disabilities Act of 1990 (ADA) an individual with a disability is a person who: Has a physical or mental impairment that substantially limits one or more major life activities; has a record of such an impairment, or is regarded as having such an impairment (Disability Discrimination).
Tinnitus
With that being said, let’s look at ringing of the ears, or tinnitus. Do you suffer from this condition? I did, and I suffered for over a decade with it. I had workups, saw specialists, had testing in a chamber that spun me around, had my ears filled with ice cold fluid, and had brain MRIs with gadolinium (a heavy metal) contrast.
I saw my primary care physician and multiple otolaryngologists including those in a specialty hearing center, none of whom could help me.
An otolaryngologist is a doctor with speciality training in treating conditions that affect the ears, nose, and throat, as well as head and neck surgery. The complete specialty is really otorhinolaryngology, which includes diseases of the nose. After college, this type of medical training includes 4 years of medical school followed by 5 years of specialty training.
Why is Tinnitus An Invisible Disability?
The hearing disturbance of tinnitus poses a significant emotional challenge to the sufferer, who perceives alone in his or her solitary battle. The fight is constant and alone, seemingly with little to no help in the initial stages of the disease.
Tinnitus changes perception, becoming a constant, underlying nuisance.
Workups take time, insurance referrals may be painstakingly slow, and the effort may become a part-time job.
In contrast to physically visible disabilities, the loved ones closest to the patient with tinnitus typically has a difficulty acknowledging or understanding the situation’s severity. They may actually “forget” that the tinnitus is always there.
Difficult adjustments must be made by the sufferer, who suffers in silence. These add an increase in additional co-morbidities.
The Co-Morbidities of Tinnitus
Social: The patient may avoid loud surroundings that aggravate tinnitus, and/or avoid going out at all. The patient may be more irritable, suffer insomnia, or be so distracted by the tinnitus that they cannot concentrate on a conversation.
Professional: Patients may be distracted by the tinnitus so much that concentration and focus are adversely and significantly affected.
Insomnia. About 66-76% of tinnitus sufferers face sleep disturbances. When everything in the house quiets down, the tinnitus “phantom noise” is amplified.
The amplified tinnitus can seriously disturb sleep with an inability to fall asleep, stay asleep, or early awakening, and disturbances of the sleep-wake cycle. Brain wave evaluation shows that tinnitus may cause patients to stay in the “shallow sleep” phase, preventing deep, resting sleep. Without good sleep, concentration and focus may be adversely affected.
Attention Deficit can occur in varying degrees. In mild cases, the patient can manage work with limited efficiency. As it worsens, focus on one task is lost, and work ability is limited. In the most severe forms, tinnitus becomes a disability, with adverse effects on focus, orientation of time and space, and understanding of the task at hand. Behavioral therapy may be a good treatment plan for any invisible disability affecting one’s job.
Psychological: The patient may feel like they are going crazy, having trouble finding someone to talk to (who understands), and/or losing sleep, becoming progressively more anxious and depressed.
Irritability. This can affect all areas of life, from personal to professional. While irritability is understandable, it may be compounded by fluctuating tinnitus, where symptoms undergo crescendos and decrescendos that not only lead to annoying immediate effects, but an apprehension for fear of an imminent recurrence.
Chronic fatigue. Constant noise, insomnia, and attention deficit may lead to chronic fatigue, further compromising professional and personal work and relationships, respectively, and predictably, worsening tinnitus.
Relationship Strain. Patients may either be constantly talking about their condition, or reluctant to talk about it. Partners may not manage the patients’ mood swings, attention deficit, or irritability.
Somatoform Disorder: Mysterious bodily symptoms like pain or aches may pop up, those are medically unexplained. This association of tinnitus with somatoform disorder is 42%, with an unexplained tinnitus being more linked to this disorder.
Cognitive Disorder: The annoyance of tinnitus can take away a chunk of brain power that could be used for normal activities like memory building. Because chronic tinnitus affects information perception, memory can be “lost” if it was never stored. Patients can report trouble retrieving memory information, because they had poor concentration in storing the information in the first place. Additional cognitive functions can be adversely affected, including general intellect, problem solving skills, and focus. Tinnitus can therefore be likened to neurodegenerative disease and dementia, without a brain injury proper, but with similar effects on memory.
Anxiety: Compromised personal and social functioning may be so compromised that patients lose confidence in their resilience and develop constant fear of new surroundings or situations. Patients may possess a constant feeling of being judged, or have self-depreciation or self-doubt.
Depression. The patient may avoid activities that they once enjoyed. Daily life may become an overwhelming challenge.
Interestingly, environmental sounds that match the frequency range of the patient’s tinnitus can also lead to mood swings. Remember this, because in future articles, we will discuss the “frequency” of light waves, energy fields, and more.
Symptoms of Tinnitus
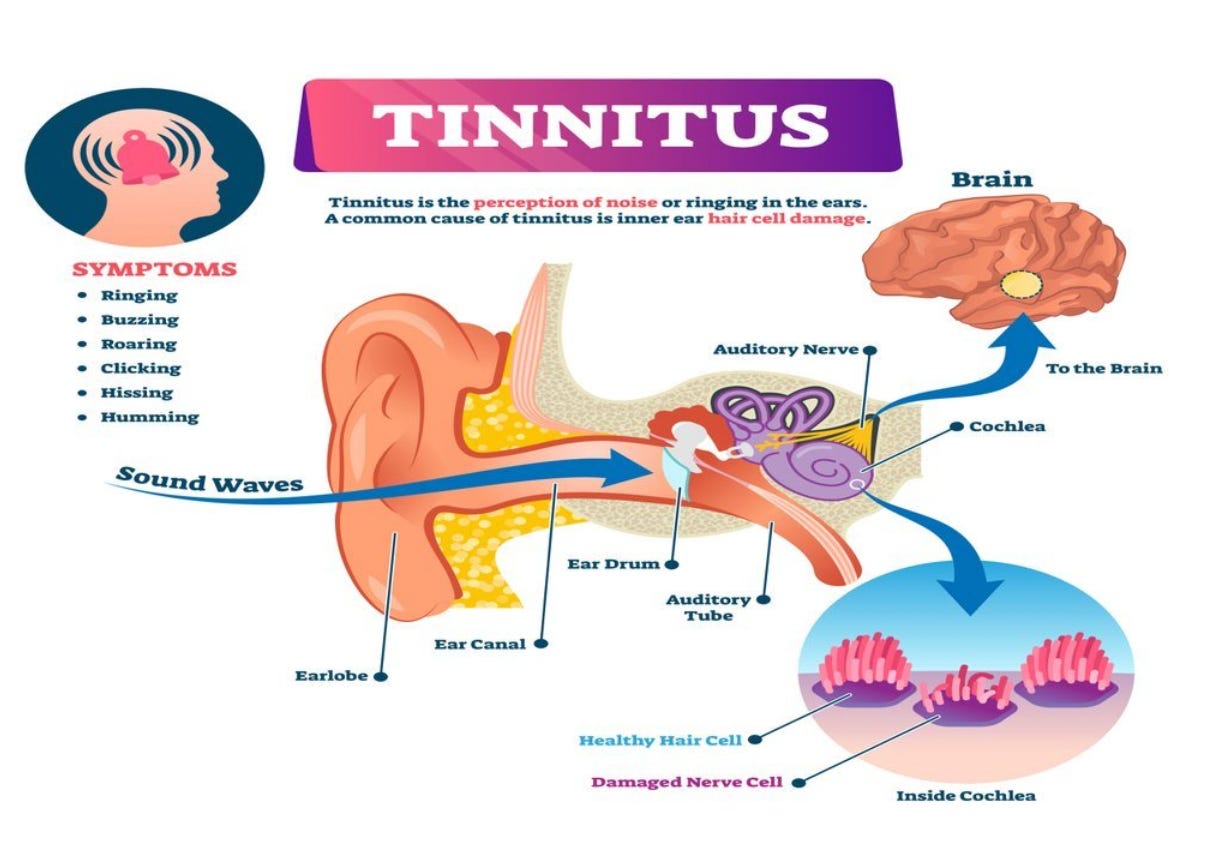
Tinnitus is defined as a perception of tonal variations that can’t be traced to an external oscillatory source. Symptoms include adverse sounds that eminate from either one or both ears.
When the ears hear ringing, buzzing, clicking, roaring, hissing, buzzing, or and/or fizzing noises, that can overpower the sound of a bar football game. Tinnitus may not sound like “much”, but is is a problem.
For the sufferer, it is as if their ears are 10 times too big for their head. But they don’t hear loud “everything” - they just hear loud “buzzing”, “ringing”, or “fizzing” noises that make one pause.

The Concern About Tinnitus
Due to the draining, nonstop ringing sounds, tinnitus can become a VERY pressing concern.
Some with tinnitus even consider suicide.
The noise is that bad.
That is the biggest concern, especially if the patient feels minimized.
The Incidence of Tinnitus
Simply Health Today estimates on the incidence of tinnitus can be found here (my emphases in bold):
More than 50 million Americans suffer from some degree of tinnitus.
16 million Americans experience such severe ringing that they require some type of treatment, and
Another 2 million suffer from such debilitating tinnitus that it impacts their daily lives.

The Anatomy and Physiology of Tinnitus
Of course, tinnitus can be a symptom of something not simply “sound” related, in that it can be a result of a problem with an anatomical hearing component.
Anatomy
To understand all the different causes of tinnitus, let’s look at the anatomy of the ear. Here is a diagram by BetaHealthy.com:
Sound waves travel through the outer ear to the inner ear, then to the brain. Damaged hair and nerve cells inside the structure called the cochlea, are implicated.
Physiology
Sound is perceived by our brains when sound wave oscillations from outside the ear go inside the ear and then are conducted as electrical signals in the neural pathways to the brain (i.e., the hammer, anvil and stirrup and associated nerves), where they are then perceived by the brain as an integration with the meaning of the sound.
One-Sided Versus Bilateral Tinnitus
Left-sided hearing loss can present with left-sided tinnitus.
Also, the frequency range, i.e., low- versus high-frequency ranges, may reflect unilateral or bilateral tinnitus. A “low-frequency” hearing loss may occur with a ‘buzzing” type of tinnitus.
This inter-relationship of frequency and one-sided tinnitus means that treating this type of hearing loss in one affected ear may occur by placing a cochlear implant.
Two Main Types of Tinnitus: Subjective and Objective
Subjective tinnitus occurs from a disruption in the electrical or neural conduction pathways (in the neurons or the nucleus in the brain), where sound is perceived. It is an issue of brain-derived, nervous tissue. Abnormal electrical currents in these pathways may show up as ringing in the ears. “Subjective” is as interpreted by the hearer; the examiner cannot hear the sound. This is usually a measure of cochlear damage.
Objective tinnitus has an actual oscillatory source that makes vibrations close to the ear’s sensory apparati. Here, minor muscle and bone vibrations from the inner ear (i.e., not from an external or visible source), are conducted to the brain and cause a “ringing” or other tinnitus pattern. “Objective” is numerical data, not subject to the hearer’s interpretation.
The Differential Diagnosis of Tinnitus
Tinnitus can be a presenting symptoms of something else like a brain tumor. The list of diagnoses that a symptom can be a sign of is called a “differential diagnosis” or “DDx” for short, often written in medical notes.
We can break up the cause of tinnitus into two categories: acute or chronic. “Acute” means that it just happened suddenly; “chronic” means it is long-standing. We can also do our differential diagnosis by starting with the most common causes and/or the most worrisome.

The Differential Diagnosis of Tinnitus Includes:
Senile Hearing Loss. Interestingly, with hearing loss, it is thought that the brain makes up for sound deprivation by the perception of ringing in the ears. Hearing loss with advanced age is called presbycusis. In an estimated 90% of cases, tinnitus coexists with hearing loss. At age 60 - 69 years, the incidence of tinnitus peaks at 14%.
Noise. Noise is a significant factor that can cause either acute or chronic tinnitus. Acutely, a very sudden exposure to noise can cause a short-lived tinnitus, like attending a loud concert. As with walking out of a concert, eliminating the noise source can stop the tinnitus, or it may be short-lived for 24 hours or less. Differently, chronic tinnitus from noise exposure can gradually become more and more intense; it is usually a high pitch, and can be intermittent or constant. This type is seen with partial hearing loss.
Ear Wax. Wax buildup can cause impaction, complete ear blockage, and tinnitus. Often after a professional disimpaction, tinnitus may worsen before getting better.
Meniere’s Disease. This is an inner ear problem with tinnitus as a less common first symptom. The most common symptom is imbalance, unsteadiness, or vertigo, sometimes accompanied by hearing loss and a feeling of having a full ear. Tinnitus due to Meniere’s disease is only clinically important in about 19% of total patients, and is high on the list of probabilities when tinnitus occurs together with imbalance. The sound of tinnitus is described as a low frequency type, not constant but fluctuating - this makes it tolerable in initial stages but it can worsen with time.
Otitis Media. Most common in toddlers who get repetitive ear infections in the middle ear, a bacteria or virus causes a middle ear infection. The most common presenting symptom of ear pain requires an otoscope exam in person, with visualizatio nof swelling, redness, and fluid accumulation seen on the eardrum. Most commonly, both the infection and tinnitus simultaneously resolve.
Otosclerosis. A disorder of the middle ear, tiny ear ossicles undergo an abnormal transformation into spongy bone. The bone becomes fixated, interrupts sound conduction, and causes deafness. Tinnitus can also occur, as the brain compensates for the hearing loss of sound deprivation. This type can be corrected by surgery, also alleviating tinnitus. However, post-operative tinnitus from surgical trauma may be a complication.
Cardiovascular Disorders. Cardiovascular disorders cause fluctuations in the blood flow, heart rate and breathing. Any arterial damage affects the rate of blood flow, and disrupts th oxygen supply in various areas, with growth and regeneration problems. The lack of oxygen supply also decreases the replication and production of hair cells, which are of prime importance.
Pregnancy. One of three pregnant women may develop tinnitus or hearing loss due to an increase in blood volume or blood pressure, or hormonal fluctuations of progesterone.
Benign Brain Tumors. In a nationwide, population-based secondary cohert study of young and middle-aged adults, it was shown that tinnitus is associated with a higher risk of benign brain tumors. Most get an MRI to rule this out.
Headache or Migraines. Both tinnitus and headaches/migraines can be a subjective finding, i.e., a malfunction of neural pathways.
Ototoxic Medications. Hundreds of medications are toxic to the ear, i.e., ototoxic. But remember that just because a medication can cause tinnitus doesn’t mean it will. including:
Aspirin: usually cause a high-pitched tinnitus by interfering with neural brain pathways or cochlear signal transmission.
NSAIDS: ibuprofen (Motrin, Advil); naproxen (Aleve). This is usually reversible.
Benzodiazepines: Alprazolam (Xanax), diazepam (Valium), and lorazepam (Ativan).
Anxiolytic drugs and anti-depressants: amitriptyline and nortriptyline (Pamelor); antidepressants, selective serotonin reuptake inhibitors, or SSRIs (sertraline, escitalopram).
Antibiotics: Gentamicin and tobramycin (Tobrex), Azithromycin (Zithromax or the Z-Pak) and clarithromycin; ciprofloxacin (Cipro), moxifloxacin (Avelox), erythromycin and macrolide antibiotics, fluroquinolones.
See GoodRx for a list of ototoxic pharmacologics: https://www.goodrx.com/drugs/side-effects/these-11-prescriptions-may-cause-ringing-in-the-ears
Traumatic Brain Injury (TBI). Twice, I suffered a traumatic brain injury (TBI) with diabetes insipidus (DI). Both times, my tinnitus was so bad that it was incapacitating. Twelve years later, it was gone.
High Blood Pressure (Hypertension). Sound patterns may correspond to an artery near the ear, and be heard as a “whooshing” sound. On the other hand, antihypertension medications can cause tinnitus, with hypertension found in 44% of all tinnitus patients. Some loop diuretics for high blood pressure can be ototoxic, and hypertension of pregnancy is the most common cause of pregnancy-associated tinnitus, a condition known as preeclampsia.
Smokers. Smokers are at a higher risk for getting tinnitus. Nicotine disrupts the transmission of signals from the brain to the cochlea, by damaging the auditory nerve. Smoking also causes frequent ear infections in middle ears and Eustachian tubes. Smoking not only risks the life of smokers, but others near them too. Passive smoking also results in ear infection such as swelling, blockage, damage in the Eustachian tube.
Vascular Anomalies of the Head and Neck. These are usually pulsatile, thobbing with the heart beat. Vibrations through the bone can originate from a brain aneurysm or other anomalies like blood vessel tumors, or malpositioned carotid artery blood vessels, as well as or the jugular veins.
Hereditary. Bilateral (i.e., both ears, versus unilateral, on one side) tinnitus may be hereditary.
Muscular Tinnitus. In this very rare form of tinnitus, muscles around or inside the ears contract, producing a “clicking” sound. Two muscles inside the ears, the stapedius and tensor tympani are implicated, as they attach to the inner ear bones, producing clicking sounds upon contraction, usually seen after long term noise exposure.
Cerebrovascular Accident (CVA or Stroke). A lack of oxygen supply to the brain can cause a brain stroke. Tinnitus can be a result of either uncontrolled hearing functions, uncontrolled messages sent to the ears, or a dislocation of oscicles.
The Diagnosis of Tinnitus
Grade 1: No tinnitus
Grade 2: Mild tinnitus, intermittent and is only heard in silent settings
Grade 3: Moderate tinnitus, frequent in occurrence and is heard almost daily
Grade 4: Severe tinnitus, persisten, and hampers work and sleep
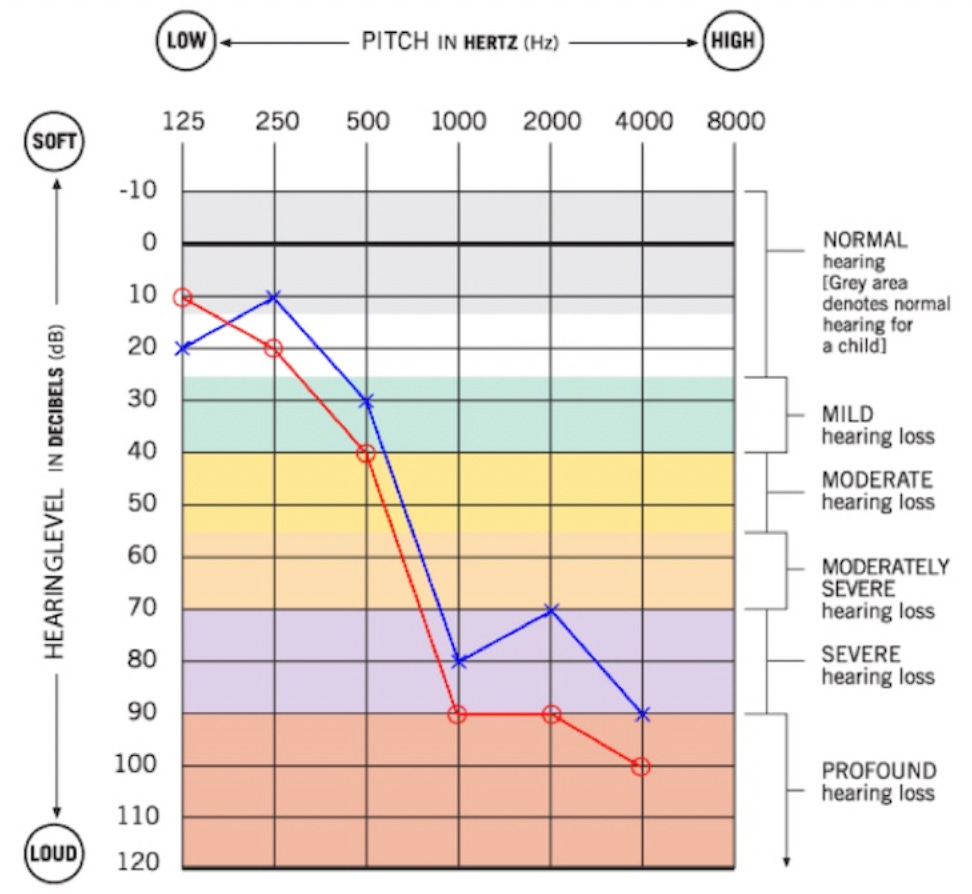
Hearing Tests
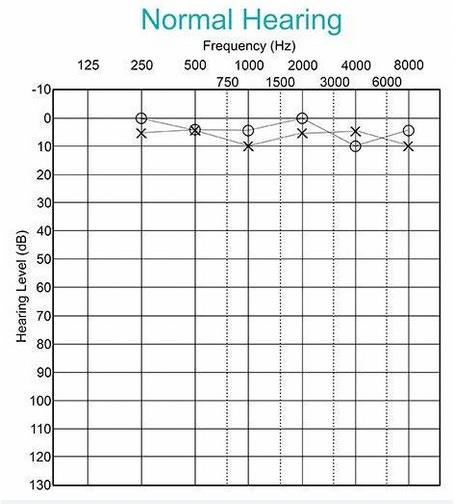
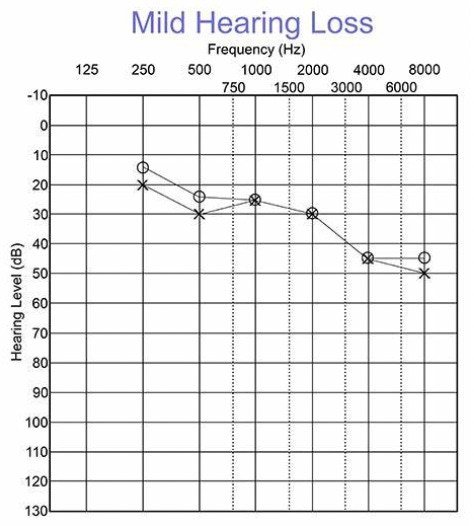
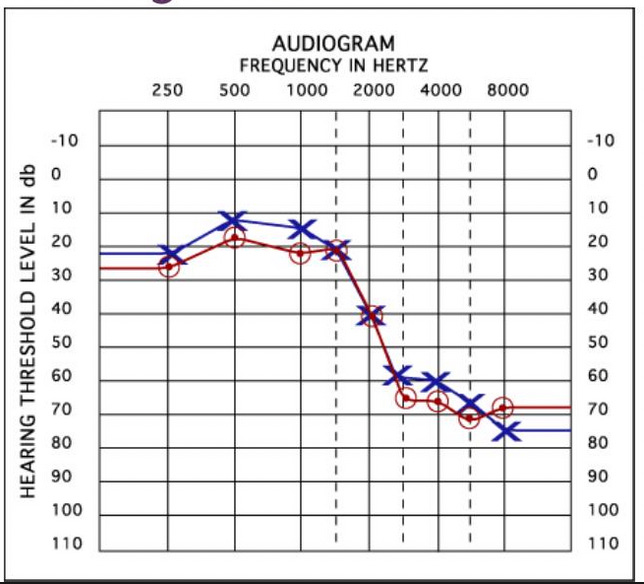
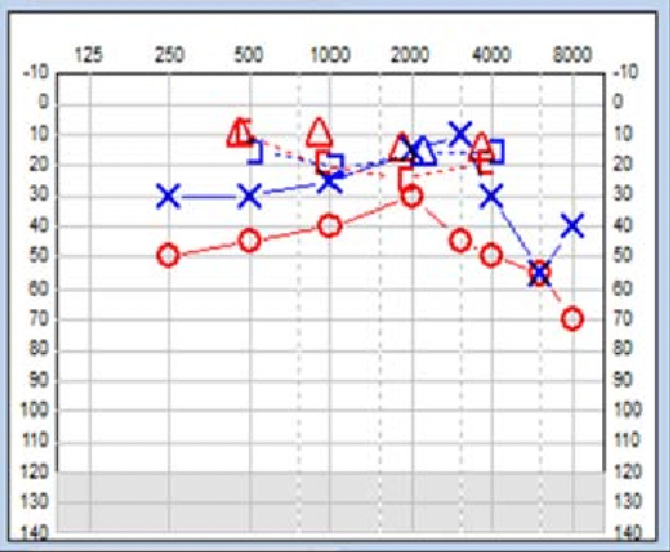
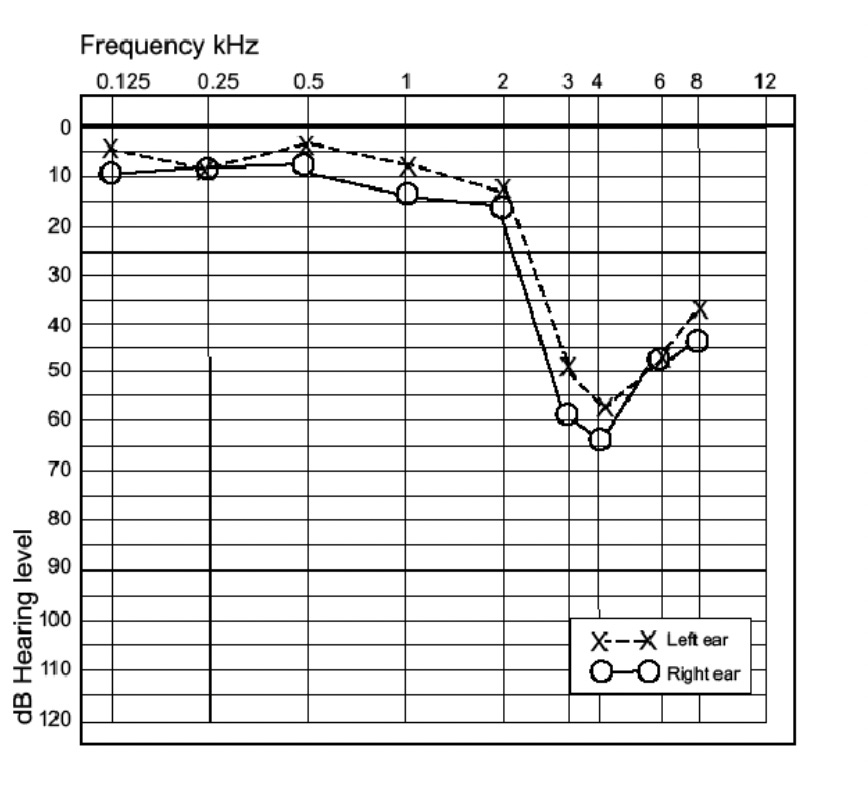
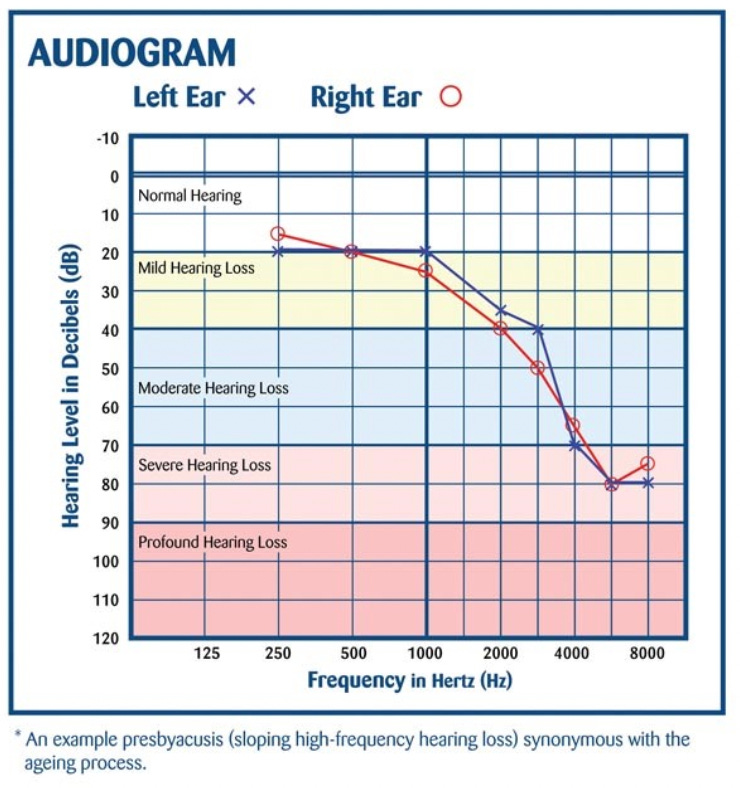
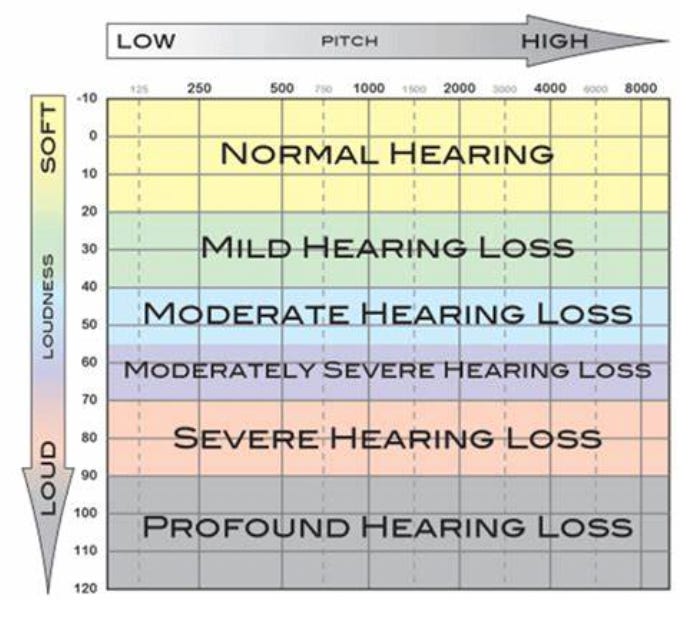
A hearing test or audiogram, occurs in a closed room. You click a button when you hear a noise through a headset, and the results are graphed, as below: See sample audiograms, below:
Based on hearing test results, the degree of hearing loss can be plotted on a graph. | Image Courtesy: https://a.storyblok.com/f/45415/1200x676/a992607077/audiogram.jpg
Above Image Courtesy: BabyHearing.com
Above Image Courtesy: BabyHearing.com
Above: Severe Hearing Loss. | Image Courtesy: SlideServe.com
Above: Moderate conductive hearing loss. Image Courtesy: ResearchGate.net
Above Image Courtesy: NationalHearingTest.com
If you have tinnitus, get a hearing test.
The Sounds of Tinnitus
Pulsatile: a vascular anomaly
High pitched: agin or noise-related
Low-pitched tinnitus: early Meniere’s disease
Clicking sounds: muscular contractions near the sensory organ of the ear
If you have tinnitus or know someone who does, I hope this article helps you understand that it may be a small word, but tinnitus is a large problem for the person who has it. It can change one’s outlook on life, leading to concentration, processing, and attention deficits.
The Evaluation and Diagnosis of Tinnitus
An ear exam: for impacted ear wax, middle ear infection, perforated eardrum.
Tone audiometry: an audiologist plays tones and then asks the patient if they can hear them. Results are shown on an audiogram.
Impedance audiometry: checks the status of the tympanic membrane and middle ear.
Speech audiometry: used for hearing aid fitting and the diagnosis of retrocochlear pathologies like tumour of the auditory nerve, auditory neuropathy, and more. Tests both peripheral and central systems.
Tympanometry: Can detect fluid in the middle ear, a perforated ear drum, impacted ear wax, scarring of tympanic membrane, lack of contact between the conduction bones of the middle ear, a middle ear tumor.
Videonystagmography or balance test (ENG): to determine the cause of dizziness or vertigo
Electrocochleography (ECOG): for Ménière's Disease or perilymphatic fistula.
Brainstem auditory evoked response audiometry (BAER, BSER): auditory nerve and auditory brain stem function.
Vestibular evoked myogenic potentials (VEMP): Superior semicircular canal dehiscence, perilymphatic fistula, Meniere’s Disease
If you have an invisible disability, you can wear a lanyard ID to show you need help at an airport or while traveling:
Order an Invisible Disabilities® ID CARD: https://bit.ly/3GHBo9B from IDA®.
The Treatment of Tinnitus
After a physical exam and testing with evaluation, the cause and treatment of tinnitus can be narrowed down.
Diet: For me, diet is always #1. Maintain adequate zinc levels, as it helps with both healing and hearing - and it is a protective factor in tinnitus. Dietary sources include dark chocolate, oysters, meat, and spinach. Vitamin B12: is found in meat and eggs. Folate alleviates tinnitus by controlling blood pressure. Natural sources include green vegetables and beans. Potassium regulates electrical conduction in all nerves, and maintains blood fluidity. Apples, apricots, papayas and yoghurt are good sources.
Ancient, Traditional Herbs: Ginseng: Used in Chinese culture, it is thought to cure hearing loss and tinnitus, perhaps via its antioxidant properties. Garlic: stabilizes blood pressure and is antioxidan. Gushen Pianas: this is a traditional Chinese herbal medicine for tinnitus.
Promote Sleep. Stop the computer before bedtime. Have a bedtime habit of taking an epsom salt bath, listening to music by candle, avoiding the cell phone and computer with its direct field of blue light, that activates the brain and opposes sleep. Keep lights off during the night, and no TV in the room.
Ear Plugs. Avoid loud noise, use ear plugs or stay away from loud noises.
Avoid Alcohol. Alcohol damages innere ear hair cells. It also damages the auditory complex of the brain, which is responsible for hearing. It can also increase both blood pressure and heart rate, aggravating tinnitus. Alcohol promotes hearing loss and damages the body’s balance controls.
Stop Smoking. Smoking causes tinnitus and makes it worse. Due to its abiity to lower the blood oxygen level, smoking damages the auditory pathway and destroys the inner ear auditory hair cells.
Hypertension: control blood pressure by weight loss, stress relief, medications that do not cause ototoxicity (ear damage).
Otoscleorosis: surgery to alleviate a fixated middle ear bone.
Ear wax: cleaning the ear, consider a professional treatment.
Hearing loss: a hearing aid; no longer is a prescription required.
Stress: Behavioral therapy targets the stress of symptoms. It can modify the emotional response, optimizing coping strategies. The primary target is to improve cognitive skills and allows a patient to exhibit a diminished response to the tinnitus. This can include relaxation and other exercises to eliminate the negative thought processes.
Mask the Sound. For me, no pathology was found and I was left to fend for myself. I tried a myriad of ways to “drown out” the tinnitus, and for short and progressively longer time periods, I could forget I had it. Strategies allow some relief from tinnitus, building confidence and stress alleviation that it is without relief. In time, longer and longer resting periods away from tinnitus can be accomplished, leading to improved quality of life and better relationships. Forms include:
Ambient sound devices: a clock or TV channel with the sound of rain, “white noise”, a tropical forest, the ocean, birds, and more. This helped me the most.
Forest sounds provide white noise and distract the brain from tinnitus. Photo by kazuend on Unsplash Modified sounds that filter the tinnitus. These devices use tonal frequencies that match the specific tinnitus tone or pattern such that the tinnitus becomes inaudible.
Modified hearing aids with sound therapy: features modified sound, as above.
Neuromodulation or Brain Stimulation. This non-invasive procedure stimulates specific brain or neuron areas in the circuit. Used for pain reduction, this increases brain stimulation in multiple regions, drowning out the tinnitus. Similarly, similar frequency waves can be delivered, interrupting the tinnitus such that it is less annoying. This is available in headphones, having a component that sends electrical signals to the vagus and hypoglossal nerves of the tongue. This treatment may be effective in 75% of patients. It is believed to be the best treatment science has come up with to cure tinnitus (Reference here).
Habituation: With this simple maneuver, tinnitus becomes more tolerable, eventually diminishing over time. I think this happened to me, with small periods of relief found by going to the beach or watching a movie. For longer and longer periods, my brain stopped registering tinnitus as being a nuisance.
Medications. There are no FDA-approved tinnitus drugs. Patients sometimes use drugs for the other side effects like depression, anxiety, and insomnia, including anti-depressants, anxiolytics, and sleeping pills, respectively. Off-label drugs include anticonvulsants and antihistamines. Antihistamines were extremely helpful to me, and I used at least two different types at the same time, because I also had Mast Cell Activation Syndrome (MCAS).
Homeopathic Remedies. Include:
Kali Mur: Used for congestion and ear, nose, and throat problems, this uses sylvine mixed with lactose sugar, which is turned into tablets.
Natrum Salicylicum: Used primarily for ear complaints including tinnitus and Meniere’s Disease, it is derived from sodium salicylate.
Chininum sulph: Used for tinnitus and Meniere’s Disease, it is derived from sulphate of quinine, and also called quinine sulphate.
Graphites naturalis: Prepared from black lead, its primary use is for tinnitus.
Avoid Triggers: This includes an avoidance of both silence and noise, stress, high blood pressure, altitude changes, alcohol, smoking, caffeine and ototoxic medications like aspirin.
Epsom Salt Foot Baths: This is pure magnesium, a natural relaxant and blood vessel dilator that has a good reputation of being relieving for tinnitus.
Yoga: With white noise as background, positions that help include the triangle pose, cobra pose, downward-facing dog, cow-face pose, and legs up the wall. I think elevating my legs helped many different things and eventually, my tinnitus all but went away. Sometimes it kicks in, but it is so rare that I cannot recall the last episode.
Accupuncture: Recommended for a variety of ear, nose and throat ailments, clinical trials show a placebo effect for tinnitus; it alleviates anxiety, improves blood flow, and is generally beneficial for many who prefer ancient medicine.
Meditation: May help with ambient white noise, stress alleviation, and more.
References
Consider Donating to The Invisible Disabilities Association®