Postural orthostatic tachycardia syndrome (PoTS or POTS) is a dysautonomia. Some use the terms interchangeably. It is a heart and blood vessel complication suffered by many after a virus infection, including Long COVID.
Depicted in old films having a young woman who lives in a day bed and constantly faints into the arms of her knight, it is likely synonymous with the term "The Soldier's Heart" coined by Sir James Mackenzie in 1916 (Kavi, 2012) was only defined as PoTS per se in 1993 (Raj, 2020).
The brain needs to get blood in order for it to get its own oxygen supply. If something happens to compromise the blood supply to the brain (and thus the oxygen supply), the body automatically compensates for it. God-given compensation mechanisms are triggered, and the body tries harder and harder to prevent the brain from losing oxygen. This is the basis of POTS: the math of the brain.

To understand POTS, one must first understand both the nervous and the circulatory systems.
The Nervous System
This is comprised of 1) the central nervous system: brain and spinal cord, and 2) the peripheral nervous system: all the nerves from the spinal cord going to and from the muscles (i.e., peripheral nerves to the arms and leg muscles) and visceral organs (i.e., autonomic nerves to the stomach and heart).
The nervous system is "automatic". Nothing controlled by the autonomic nervous system happens with the deliberate mind. It encompasses such things the blood pressure, heart rate, food digestion, the motility of the stomach and intestines, the production and elimination of urine and feces, sexual organs and reflexes.
Dysautonomia/POTS
Dysautonomia is "dysfunction" of the "automatic" or "autonomic" nervous system. The dysregulation prevents calf veins from constricting and tightening up to squeeze blood up to the brain when you stand up. When the brain does not receive enough blood supply when going from laying to standing, or from kneeling to standing, it sends out "autonomic" or "automatic" signals crying for help to save itself. It tries to pump more blood to itself. If it fails, the person faints.
The Circulatory System
With dysautonomia, one gets lightheaded when standing up. A patient feels like she is not getting enough oxygen to the brain, when the fact is that she are not getting enough oxygen to the brain because she is not getting enough blood supply to it.
When a patient with dysautonomia stands up, he feels dizzy because the leg veins do not "squeeze" to keep blood flow going to the brain. Instead, blood pools in the legs and may even leak out of blood vessels, creating discolored or swollen lower legs. When the blood pools in the legs, it decreases the amount of blood returning to the heart. In turn, this means that the heart is "less filled" with blood, so it pumps significantly less blood forward to the brain and other vital organs.
If very severe, the patient may actually faint or have a "gray-out" that is close to fainting, or syncope. This condition can be aggravated by position changes such as standing, not eating enough salt, not drinking enough fluids, sweating too much, or being in a hot environment.
Each case of POTS is unique. Symptoms may come and go over a period of years. In most cases, symptoms are alleviated with diet, medications and altered physical activity. Symptoms may completely subside if an underlying cause is found and treated.
Forms of POTS
Neuropathic POTS: Peripheral denervation (loss of nerve function) causes poor blood vessels in the muscles, especially in the legs and core body.
Hyperadrenergic POTS: Overactivity of the sympathetic nervous system.
Low blood volume POTS: Reduced blood volume can lead to POTS. Low blood volume can cause similar symptoms that may overlap in neuropathic and hyperadrenergic POTS.
Risk Factors
Most POTS patients are women aged 13-50 years. About 1 - 3 million people suffer from POTS in the United States.
It can develop after a viral illness like COVID, serious infections, any other medical illness, pregnancy, and trauma such as head injury. It is commonly associated with Long COVID.
No one knew about POTS when I had my traumatic brain injury. I could not stand up without fainting until literally 26 doctors had rolled their eyes on me, thinking I was pretending. I finally found a cardiologist who put me on a Tilt Table and I promptly passed out, confirming the diagnosis. It was a barbaric way to get the diagnosis, but it got me the treatment I deserved. Now it is virtually gone. So be assured that we will help you get through this!
POTS may develop after a significant illness (especially after hospitalization and prolonged immobilization). It may develop after mononucleosis. Those at higher risk of developing POTS include those with certain autoimmune conditions such as Ehlers-Danlos and associated hypermobility Syndromes (EDS) Sjogren’s syndrome, and celiac disease. EDS patients may also acquire Mast Cell Activation Syndrome, or MCAS, which is highly controlled by an antihistamine diet and antihistamines.
EDS is diagnosed by history; there is no definitive genetic test. I am an EDS expert and I refer patients to cardiology for POTS, as well as to urology for neurogenic bladder, GI for gastroparesis, and more. Sjogren’s can be evaluated by blood testing, lip biopsy, dry eye test, and a rheumatology consult. Celiac disease can be tested through blood work, GI consult, and if needed, biopsies of the small intestines. I cover EDS in my Guidebook to Low Back Pain: Diagnosis and Treatment and go over POTS, MCAS, and more.
POTS Symptoms
Symptoms can be uncomfortable, unexpected, and frightening. Patients usually have from two or more symptoms listed below:
Blood pressure. May be high or low, or change from one to the other.
Heart rate. May be high or low, or change from one to the other.
Chest pain. May be related to heart rate or blood pressure changes. May be related to a particular kind of heart failure. All patients should see a cardiologist, get and EKG and an Echocardiogram.
Dizziness or lightheadedness. Occurs upon standing, after prolonged standing in one position, or long walks.
Fainting or near-fainting. Also known as syncope, patients need to be careful when standing up or they get a severe "head rush". Some had episodes of fainting or passing out in their youth, and dysautonomia can occur in children.
Exhaustion or fatigue. Patients cannot get enough sleep. They think they have energy to do things, but they make plans and cancel them.
Abdominal. Pain, bloating, and nausea may occur, especially after eating a heavy meal. The bowels may not move food forward, so they may get full fast or get nauseated after eating.
Temperature deregulation. Patients may get too hot or too cold compared to others, and are less tolerant to heat.
Nervousness. They may have a jittery feeling or experience social anxiety from a fear of fainting in public.
Brain fog. Forgetfulness and trouble focusing may occur. This is one reason to aggressively treat or overtreat with COVID, especially with the use of fluvoxamine, to decrease the risk of getting brain fog that persists for months.
Blurred vision. Changes may necessitate a visit to an ophthalmologist but there is no known diagnosis that is a common eye problem.
Headaches. May be due to blood pressure or heart rate changes, as well as tension and stress, family relationship strain, or job loss.
Body pain and aches. A flu-like syndrome may persist.
Neck pain. May reflect stress or mechanical pain.
Insomnia. Frequent awakenings may occur from chest pain or a racing heart rate during sleep, as well as excessive sweating.
Shakiness or tremors. These may occur due to adrenaline surges.
Discoloration of feet and hands. Due to blood pooling and blood vessel abnormalities, lower extremities may turn bluish or have small blue capillaries show through; leg veins may dilate.
Exercise intolerance. Shortness of breath may occur due to tachycardia but it is important to exclude heart or lung disease such as failure or clotting, respectively.
Excessive or lack of sweating. Lack of sweating is especially concerning in hot weather; some patients need to completely avoid exposure to heat.
Diarrhea and/or constipation. A search for Crohn's disease or Irritable Bowel Syndrome may also reveal an additional gastrointestinal diagnoses. May need referral to gastroenterology.
The Math of the Brain
If you are mathematically inclined or want to learn some math of the brain's blood supply, read on. If not, you may skip this section. But I hope to explain this in a short and common-sense manner that is easy to understand. You may have to pause or read it twice, but I promise it will be worth it.
When triggered by a threat, the only way that the brain receives more blood is by a built-in mathematical equation that operates as a reflex, or automatically. The equation has to do with cardiac (heart) output (CO).
Cardiac Output
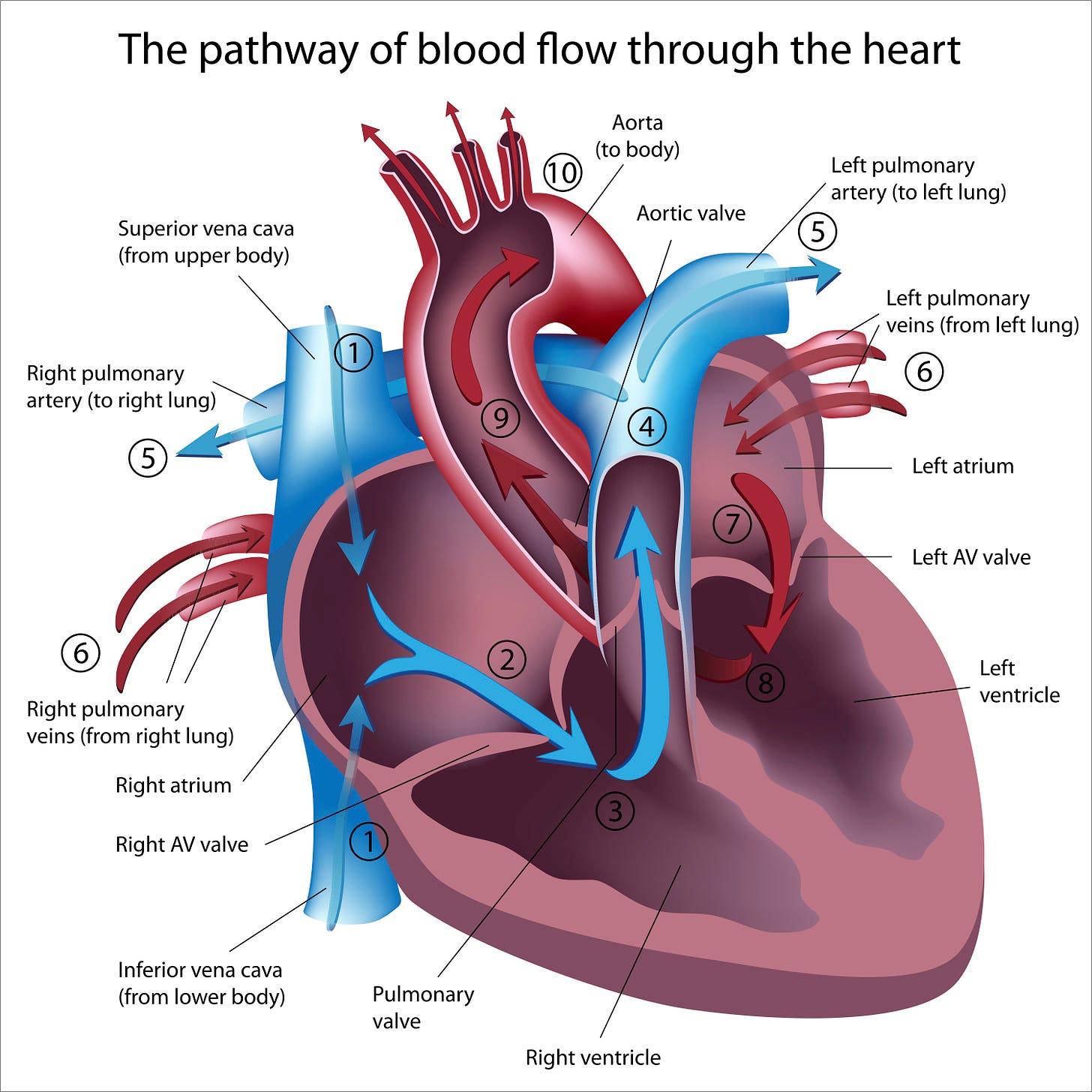
To pump blood to the body, the heart has to fill and it has to beat. With each beat, a volume of blood is delivered. This volume is termed cardiac output and there is a mathematical calculation that determines this blood flow.
The formula for this is:
CO = Heart Rate (beats per minute) x Stroke Volume (ml)
CO = HR x SV
A normal adult cardiac output is 5 liters per minute. A normal heart rate is 60-100 bpm.
Cardiac output is the amount of volume the heart pumps out through the aorta, the largest artery in the body that comes straight out of the left ventricle (see image). Cardiac output depends on two things: the heart rate and the volume of blood that is pumped out per heart beat.
The heart can't pump blood out unless it received blood into it, maintaining circulation. Therefore, it makes sense that the stroke volume depends on venous return or the amount of blood going into the heart for recirculation. In a perfect heart, venous return equals cardiac output: what goes in, comes out.
The force of contraction is another factor determining stroke volume. If the heart contracts to squeeze blood out with a lot of force, stroke volume and cardiac output increase. If a person has heart failure or a "weak heart", it does not eject enough blood with each beat.
This is the defect in dysautonomia: lack of blood returning to the heart, partly because it's pooling in the legs and partly because the blood volume is not large enough to return enough blood to the heart.
If you are dehydrated or lost blood, you have less blood volume or stroke volume, in ml/minute. The body compensates for this by increasing heart rate. If your heart rate is too slow, it is providing less volume per minute, so the body compensates by increasing stroke volume. Failures in both mechanisms lead to syncope or fainting. To keep blood going to the brain, one factor compensates for another in a positive feedback loop.
If your heart rate is too low, the stroke volume has to increase so the brain gets enough blood. If your stroke volume is too low, the heart rate has to increase to maintain cardiac output. With POTS, leg pooling of blood means the volume is low, so less is delivered to the heart, less goes out, the brain cries for help, and the heart rate goes up.
During loss of blood, dehydration, and POTS, blood volume is low and the heart may compensate by increasing its heart rate. Hence, the orthostatic hypotension, i.e., low blood pressure, automatically causes the heart rate to go faster, i.e., cause tachycardia. Hence, the acronym "POTS" is named:
P = Postural: upon standing or changes in position, the patient experiences symptoms
O = Orthostatic: low blood pressure occurs because the legs pool with blood
T = Tachycardia: to compensate, the heart rate increases
S = Syndrome: this happens over and over again, usually in a predictable manner.
If you would like more information that reinforces the physiology of the heart, a good website is HERE.
If you have POTS, help your family understand you. Share this article. We need your family to understand you.
Get My FREE Guidebook to Emergency COVID Care - with Your Personal Tracker™
https:COVIDmasterplan.com - it is at the top of the page.
This is a LIMITED OFFER UNTIL OCTOBER 31, 2022. Then it is just $4.99. It contains your shopping list for supplements, prescriptions, foods, and a time schedule of what to take and when, should you get sick. This is a perfect gift if you are single or have parents who are not internet-savy. You can print it out for them - perhaps in black and white to save ink - and have them pay attention to the 7 am to 12MN schedule on last two pages of the Personal Tracker™. https://covid-kits.com/ols/products/covid-care-tracker
For Health Care Professionals: Take Steve Kirsch’s Survey
If you work in healthcare, please consider filling out Steve Kirsch’s survey. Tell your doctors and nurses. Steve posts:
You will be asked how many reportable events you've OBSERVED vs. FILED for both non-COVID and then the COVID vaccines since you first became aware of the VAERS system. A "VAERS-reportable" event is a significant adverse event that in your opinion should be reported to the VAERS system in order to allow health authorities to accurately assess the safety profile of a vaccine. Steve askss that if you are NOT a healthcare professional, do NOT fill out the survey. If you ARE a health-care professional, fill out the form here: https://airtable.com/shrQZWaacOu9j2rhh?utm_source=substack&utm_medium=email
AFFILIATE LINKS
Proceeds go directly into Aranda MD Enterprises, to help needy patients
My most frequently asked question: “When do you sleep?" https://buymeacoffee.com/dra9
How To Win In Court Without a Lawyer. My 2nd most popular question: “How do you find a good attorney?” Too few Americans know what Justice is. Too many are denied Justice in our courts. For the past 36 years Dr. Graves has been an attorney and In 1997, he started his online course to help everyone who can't afford a lawyer by giving affordable legal know-how and solid confidence to tens of thousands of people for 25 years ... good people who now are winning in court without a lawyer!winning cases by doing what this course will show YOU how to do - step-by-step, quick & easy! www.HowToWinInCourt.com?refercode=AM0060
Z-STACK™ Supplements. by Beloved Dr. Vladimir Zelenko. https://zstacklife.com/?ref=MARGARETARANDA; Use CODE "DrMargaretAranda"
Alavida™ and Epithalamin. Alavida™ Regenerating Trio. Anti-aging patch, day and night cream; the only topical product in the world with epithalamin, a hormone produced by the pineal gland. WATCH Low Level Light Therapy (LLLT):
Corganics™. Medical quality CBD with NO THC. May help pain, anxiety, depression, nausea, inflammation, topical skin disease. Capsules, sublingual liquid, and topical. Approved by dermatologists for skin conditions like psoriasis; also by oncologists for nausea. https://corganics.com - Use CODE “Aranda” (case sensitive)
ECHO H2® WATER. Bubbles hydrogen gas (H2) into water, promoting “probiotic”, anaerobic gut flora; antioxidant, improves cognitive function, optimizes gut health. Models include: portable, under-the-sink, add-to-refrigerator, filter, acid water (use to feed plants; kills bacteria and viruses so it replaces harsh chemical cleaners; add to laundry), alkaline water (use to wash vegetables, clean kitchen countertops). https://www.synergyscience.com/shop/?afmc=1ii
LifeWave™ Wearable Patch Technology. Wearable technology for pain, Glutathione, Carnosine, X39 Stem Cell Activation with GHK-Cu, Insomnia, Athletic patches and more; no medication; uses LLLT, no drugs. https://lifewave.com/margaretaranda/store/products
Please Don’t Tell Me You Don’t Take Daily Supplements!
Metagenics™ Supplements. Physician-quality, scientific ingredients for immune system optimization. https://margaretaranda.metagenics.com
My recommendation: Immune Defense Pack + Benesom melatonin (take at dusk, not bedtime)
My Patriot Supply™: Survival foods, supplies, and Prep Kits. https://bit.ly/3a82rik
JuicePlus™ - Gummies for Kids: https://aranda.juiceplus.com
Vollara™ Space Tech Air Purification: Portable space technology museum quality air purifier kills viruses, bacteria, 1200 sq ft or office. Also available in personal space models for travel, large buildings like hospitals, schools. https://www.vollara.com/margaretaranda