Have you ever sat next to a doctor on a subway, and asked for free medical advice? I can’t tell you how many times someone asked me about their back pain or headaches, searching for a new answer. I don’t mind unless I’m really tired… but many times, I am really, really tired.
This is meant to help you with your next doctor’s visit. During this pandemic, many have avoided the Emergency Room or Urgent Care... not because they wanted to, but because they were told NOT to seek care “unless your lips turn blue” or “unless you can’t breathe”. Even Emergency Medical Technicians refused to take 911 patients to the hospital, saying, “They’re not going to do anything, anyway!”
As a person, a doctor, and The Rebel Patient, I AM SORRY!
It is embarrassing to me as a professional that doctors and EMTs could be so STUPID as to not recommend a single thing to possibly HELP, instead of doing harm by telling patients to stay home and do nothing but wait for their lips to turn blue. I have NEVER said that to my patients.
You may need to advocate your own medical care (or that of a loved one) not only in the ER but in a regular doctor's office.
On our June 29, 2022 show, The DR's CORNER: Understand Your MD brought you some great ideas on how doctors think. Because if you understand how doctors think, and if you can "spoon feed" them your patient history in the form of paperwork and information, they will get to your diagnosis and treatment plan.
Without the proper diagnosis, it is impossible to get the right treatment. And because medical error is a problem, get the most out of every doctor's visit.
Dr. Margaret Aranda walks you through the scenario of every patient presentation, further described in her book, The Rebel Patient: Fight for Your Diagnosis. Taking her hard-learned lessons from fighting to get her own diagnoses of traumatic brain injury, diabetes insipidus, and dysautonomia/Postural Orthostatic Tachycardia Syndrome (POTS) her original eBook may be found here.
Stay tuned for the Revised Edition will be released in later this year, 2022!
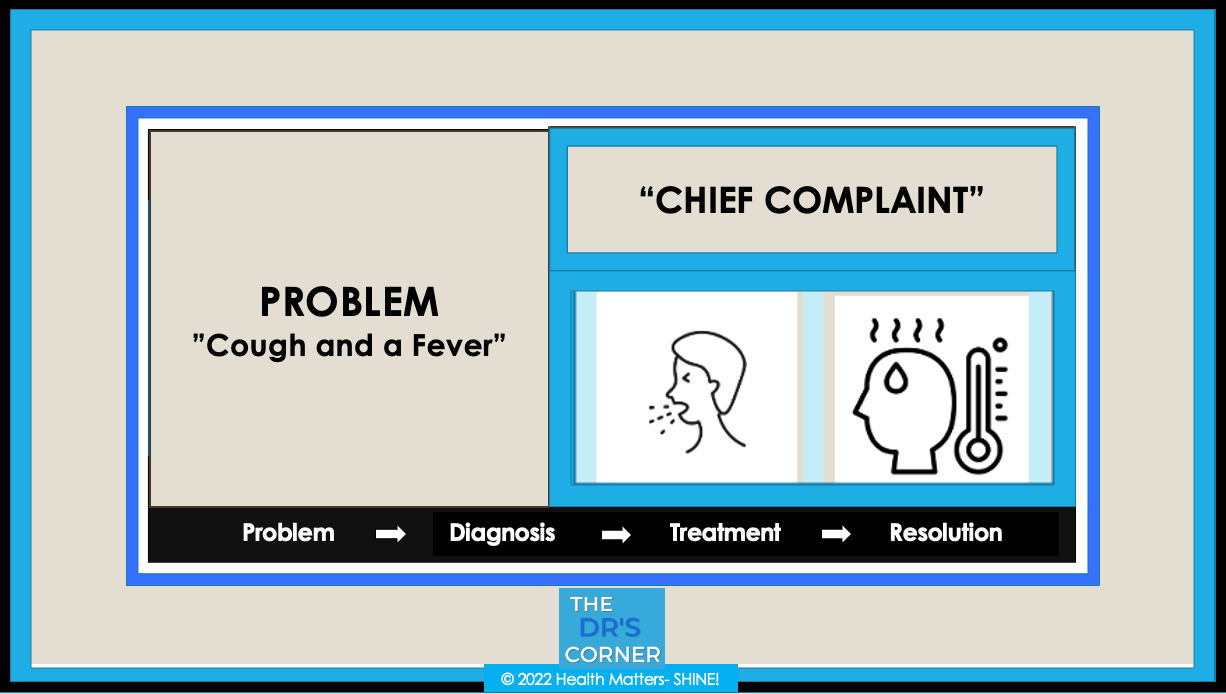
1. Chief Complaint (CC): In your words, your main complaint (see image above). Example: cough and fever.
2. Associated Symptoms: Includes additional information on the same problem: How long you have had the problem? What things did you do to treat it? Example: medications taken.
3. History of the Present Illness (HPI): Associated symptoms, like fevers and chills, other events that happened in the timeline that brought you to the doctor's visit.
All your paperwork spoon-feeds the doctor, so that she can get the right diagnosis. Be patient with her questions, and be wary of health care professionals that don't ask you questions. Since 99% of the diagnosis is in your patient history, a good doctor investigates it like an investigator investigates a crime.
The example patient presented to the ER and was told several surprising and horrific instructions, which we reviewed.
4. Past Medical History (PMHx): Your existing diagnoses, if any, such as diabetes or cancer.
5. Past Surgical History (PSHx): Your previous surgeries, if any, such as having your appendix removed.
6. Medications: Your list of supplements and prescription medications.
7. Allergies: Your list of allergies. If none, we write "N.K.D.A." = No Known Drug Allergies
8. Social History: Your history of alcohol or illicit drugs, as well as smoking history.
9. Family History: Diseases that run in your family, such as cancer or diabetes.
10. Vital Signs: Nursing staff not only evaluates your condition to give the doctor report, but also takes your vital signs.
THE VISIT: Now it is time for the doctor to see you, but only after all the above information is written and available in your chart. No chart, no paperwork = the doctor cannot see you. The doctor needs to weigh all the paperwork, consider ordering additional tests like blood work or x-rays, and consider getting a consultation from a specialist. Only then is the doctor able to arrive at your diagnosis.
PHYSICAL EXAM: A directed physical exam helps pinpoint a diagnosis. If we determined her vitals were fine, and her lungs were fine, she may not need a chest x-ray. OR, maybe she does? Watch the video and see what you would do for this patient.
TESTS AND X-RAYS: We reviewed possible chest x-ray findings, and explained several possibilities of what we could find, such as a pneumonia. We could also determine also other possibilities if they came out negative, i.e., maybe an early pneumonia or something more. If it was a negative x-ray, would you order another study? If so, what would it be? Dr. Aranda discussed the thought that go through a doctor's mind when they order any test. Then she reviews what actually happened with the example patient.
TREATMENT: Dr. Aranda reviewed the patient's actual findings. Then she reviewed COVID-19 early treatment protocols, as well as additional therapies. She also provided a Shopping List that included items to help during both the treatment and recovery phases of COVID illness.
PREVENTION: Since it is best to not get sick in the first place, Dr. Aranda reviewed prevention protocol supplements and prescription medications that may be of benefit. She included a review of how to calculate your Body Mass Index (BMI) for categorizing various stages of leanness or obesity. She reviewed some medical equipment to have in your home.
CONCLUSION: I revealed the patient's outcome.
Based on this true story, The DR's CORNER enables you to have some advocacy tools and to listen carefully and know how to best answer "Yes" or "No" questions (i.e., with a "Yes" or a "No") ~ so your doctor can best arrive to YOUR DIAGNOSIS! Then you can focus on getting the RIGHT TREATMENT!
There is no substitute for watching THE DR's CORNER: Understand Your MD! Watch here:
And if you missed Show 1: watch here:
~ ~ ~ ~ ~