What is Your Vitamin D Level? You Need to Know, as COVID is Already Back
Ask Your Doctor. If She Won't Help You, Get a New Doctor. It takes two weeks to get your vitamin D level up, so please don't tell me you don't have supplements yet!
Note: This is a reprint with significant edits, from my March 22, 2022 original article. I posted it to Substack “Notes” today, but my email audience will not receive it, so I rewrote and updated it for you.
I dedicate this article to Joe, who just today realized he has been vax injured. » » Pray for Joe, because he is sad - but he WILL GET BETTER, thank God.
Thank you also for keeping Karen Kingston in your prayers, as I know you do.
Thank you for caring about what I have to say regarding vitamin D levels.
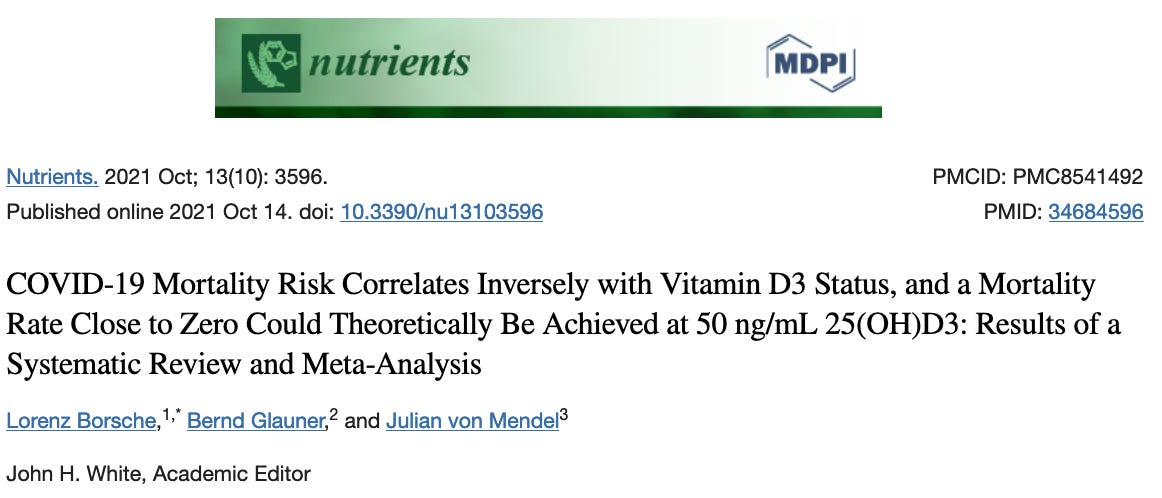
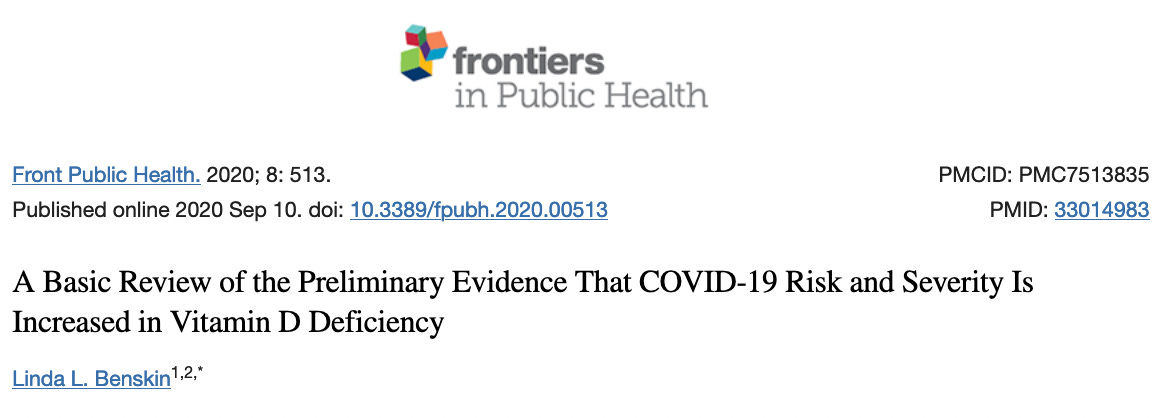
Fact. Low vitamin D3 levels have been associated with increased COVID-19 mortality. A level above 30 ng/ml may "significantly decrease mortality" and a level above 50 ng/ml "may prevent any excess mortality" from COVID-19.
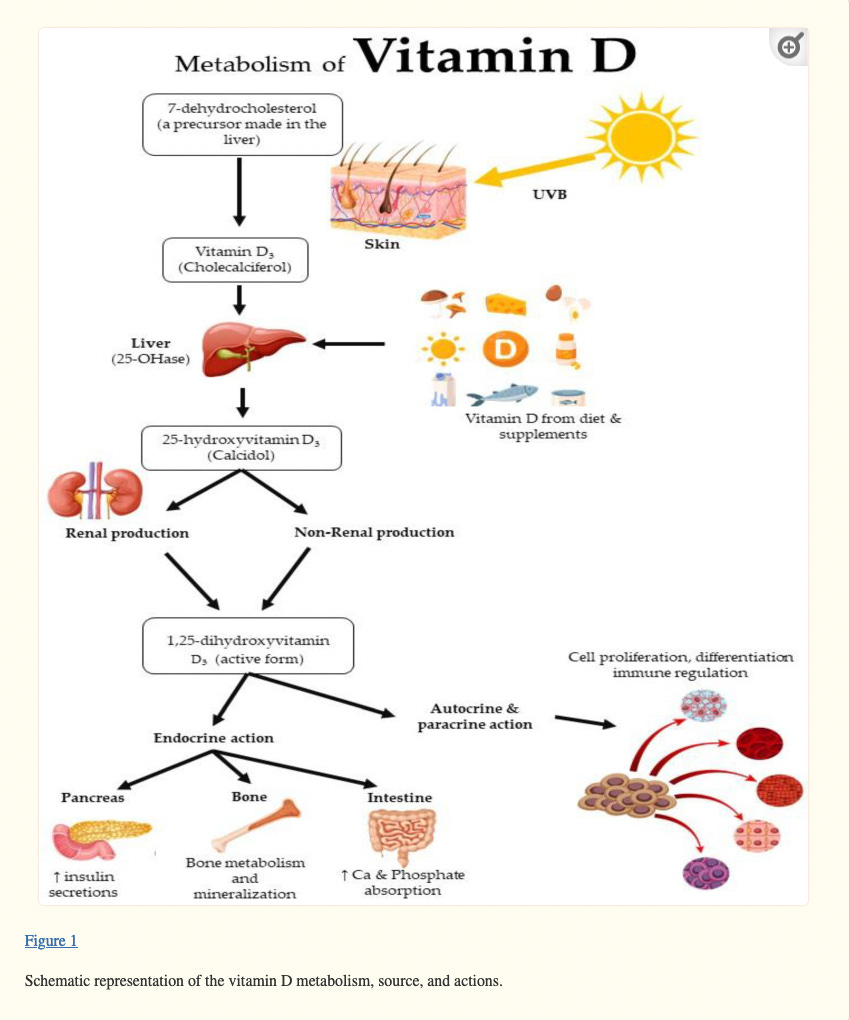
What Is Vitamin D?
Vitamin D is a fat-soluble vitamin, meaning that it is stored in fat tissue for later use. As with ivermecitn, always take your vitamin D supplement with fatty foods. The fat-soluble vitamins are A, D, E, and K.
Many doctors and pharmacists compound ivermectin and vitamin D together in a capsule; they are excellent to take together with 30 grams fat.
They Go Hand in Hand: Vitamin D and Its Deficiencies
(None of these statements are approved by the FDA and vitamin D is not a cure for any disease)
To help increase vitamin D, get more sunshine, eat the right foods, and take supplements. AND check your blood level to be sure your body is absorbing it. If you don’t have a recent blood level of vitamin D, get one this week.
Many of these correlations are found in this wonderful PubMed review*:
Bones. Low vitamin D makes it impossible to absorb all the calcium you need. It forces calcium away from your bones, making bones brittle, causing osteomalacia or “adult rickets”. This leads to bone and muscle pain. It can also cause osteoporosis, thinned bones and an increased risk of bone fracture.
Cancer. Vitamin D decreases the chance of getting these cancers: breast, colon, and prostate.
Cell growth. Optimizes cell growth.
Chronic disease. Reduces such illnesses as chronic obstructive pulmonary disease (COPD), diabetes and metabolic syndrome, heart disease, high blood pressure, and multiple sclerosis.
Chronic fatigue not relieved by any amount of sleep. Can be due to a low vitamin D.
Depression. Vitamin D deficiency can lead to depression, because vitamin D is needed for brain function. One study shows that hospitalized patients with a vitamin D less than 50 ng/ml can go into depression. Another one shows an association with depression in patients with metastatic lung cancer.
Gut health. Vitamin D regulates gut barrier function and the creation of antimicrobial peptides, which may protect against colon cancer and irritable bowel disease (IBD).
Immune system. Optimizes the immune system, keeping inflammation in check. Other supplementation that help includes vitamins C and A. With a good immune system, your body can fight infections and diseases like COVID, the flu, the common cold, and strep throat.
Low back pain. Yes, low back pain can be due to a low vitamin D level. Other associated areas include the ankles, chins, and forearms.
Lungs. Improves lung function.
Mood. Is importating in mood regulation, helping avoid anxiety and depression.
Nervous and muscular systems. Optimizes nervous system function.
* = Reference: Md Isa Z, Amsah N, Ahmad N. The Impact of Vitamin D Deficiency and Insufficiency on the Outcome of Type 2 Diabetes Mellitus Patients: A Systematic Review. Nutrients. 2023 May 15;15(10):2310. doi: 10.3390/nu15102310.
I hope this helps you see how important vitamin D is. Are you going to get a vitamin D level soon?
What to Do: Get Your Vitamin D Level Up Now, Before the Fall
Ask your doctor,
Can we check my vitamin D level?
Because you should be able to do that.
Vitamin D Levels are Associated with COVID-19 Mortality.
We want you to check your vitamin D level because it’s important.
Borsche et al, who published the above findings in Nutrients, October 2021, state a COVID-19 mortality risk close to zero could theoretically be achieved at 50 ng/ml vitamin D3. They agree vaccination is important to fight SARS-CoV-2, but encourage it should not be the only focus; the immune system should be strengthened.
What if you’re vaccinated?
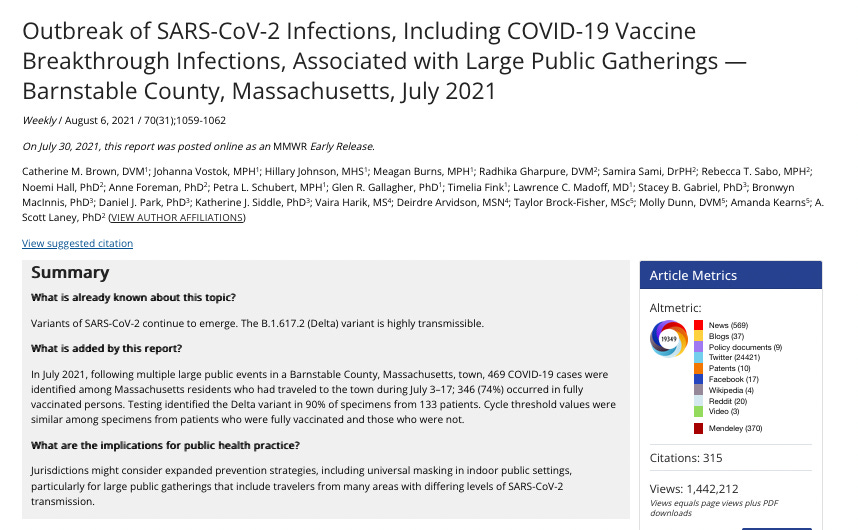
Brown et al in the MMWR Morbidity and Mortality Weekly Report of August 6, 2021 (see below), show that vaccinated people can still be infected in breakthrough infections, particularly when associated with large public gatherings. Even if you’ve been vaccinated or already had COVID once, it’s still important to know your vitamin D level.
If you get a blood draw vitamin D level, you win the prize! Everyone should know their “number”. Is it 30? 53? 75?
Many sources recommend a vitamin D level over 50 ng/dl, with or without a blood draw (the first choice is to know your actual blood level).
Get Well
Vitamin D Deficiency. First described in the 19th Century when child laborers of the Industrial Revolution working in dark warehouses got soft bones, it is unfortunate that The Endocrine Society recommendations define vitamin D deficiency at this outdated and lowest mark of 20 ng/ml, established over 100 years ago for rickets.
What vitamin D level is your doctor okay with? 20? 30? It should be over 50, and many believe it should be 70-80.
Today, the well-documented and worldwide problem of Vitamin D3 deficiency is exacerbated in the winter season due to: weather prohibiting outdoor activity, kids being back in school to bring home more viruses, plus colds and flus abound.
And we see mandates threatening to come back.
Recommendation: First, get your vitamin D level checked, to know what your "number" is (or not, and “guess-timate” it) , then replace with high-dose vitamin D.
» Scenario: You got your blood drawn and are now in your doctor’s appointment«
Your Doctor’s Appointment
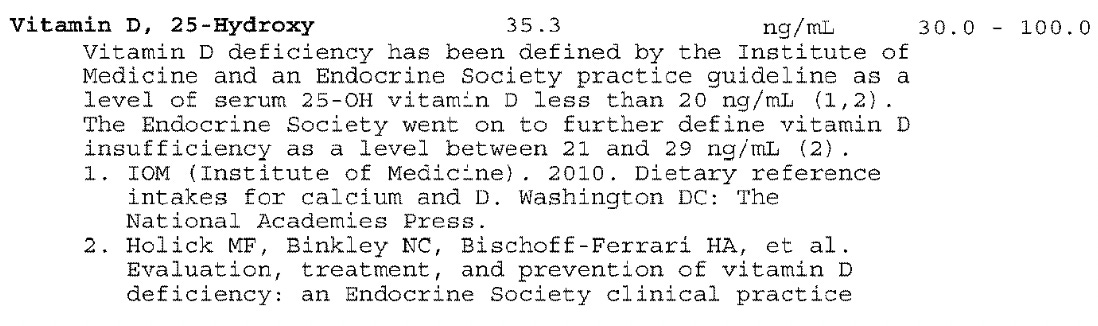
Your Vitamin D Level. At your doctor’s appointment, we both have your labs in front of us. You note the following lab value, with the normal reference range to the right:
Your vitamin D = 35.3 ng/ml. The Normal Range = 30-100.
Are you happy with this?
ANSWER: No, you should not be happy with this - we want it to be 70-80.
Discussion with Your Doctor
In the COVID climate, your goal is to have a vitamin D level over 50 but our real goal is 70-80 because it takes 2 weeks to get your level up, and then you're set in case you get sick and throw it up.
You can ask your doctor:
What do you think my vitamin D level should be? (50 or over)
Do you think it should be 35? (No)
Do you think it should be 50? 75? (Yes. I prefer 75.)
Will you prescribe me some high-dose vitamin D, like 50,000 IU a week? (Of course! We give you the risks/benefits informed consent, advise to take with fatty food.)
Considerations
If your doctor orders any lab, she is responsible for the results, including fixing anything that is wrong.
Dietary forms of vitamin D: fortified cereal and milk, fish like tuna, salmon, cod; beef, chicken, mushrooms, especially Portabella.
If your doctor doesn’t know what a normal vitamin D level is without looking, get another doctor.
If you get labs ordered by a Consultant, private insurance usually pays for it.
If your doctor doesn’t mind having a Consultant help with wellness, ask if they could work with one to help your vitamin D level get higher.
Do a vitamin D and Zinc blood draw at the same time. Zinc is necessary for the following to work by halting viral replication: quercetin, doxycycline, hydroxychloroquine and EGCG, found in green tea.
If your doctor won’t prescribe vitamin D so your level gets to be 50, ask why. Then consider getting a second opinion. You deserve the best.
If your doctor doesn’t know how much vitamin D to give after your lab results, read on.
Haven’t had any blood drawn in 2 years and you’re over 50? Consider getting additional labs.
Consider blood tests for organ systems (blood count, kidneys, liver, electrolytes), SARS-CoV-2 antibodies if you’ve been sick, blood clotting, age management (hormones, thyroid, diet), autoimmune disease, inflammatory markers, the adaptive response after vaccination, other viruses like Lyme and thyroid disease, or everything.
Don't wait until you're sick to start vitamin D. It is important for prevention and treatment of early COVID-19.
Top 3 Benefits of Vitamin D
Wide Impact on the Body. Vitamin D influences over 2500 genes, impacting dozens of serious conditions including modulating the innate and adaptive immune systems (B cells, T cells, natural killer or NK cells dendritic cells). It improves weakened or unregulated immunity and can improve diseases like virus infections, respiratory infections like ARDS, and several autoimmune diseases like multiple sclerosis. It affects such conditions as autoimmune disease and cancer.
Not Just a Vitamin: A Necessary Metabolism Hormone. Activated vitamin D3 receptor binding engages a conglomeration that forms a "vitamin D3 response element" (VDRE). Therefore, "vitamin" D is not just a vitamin; just like steroid hormones like cortisol or testosterone, it is a highly necessary hormone of equal importance to human metabolism. Some call it the “master hormone”.
COVID Severity and Recovery. COVID fatality rates tend to be worse in several patient populations who also have very low vitamin D3 levels: the elderly, African Americans, and those with co-morbidities like diabetes, obesity, heart disease, chronic inflammatory disease and cancer.
Next 3 Steps
Know your blood vitamin D level. Ask your doctor. Get your blood tested. Then take enough to keep a level over 70. If you don't know your vitamin D level, we can estimate how much you should take. If you don’t know your vitamin D level, see below (I have you covered).
Optimize wellness. Maintain a good weight, eat well, correct hormone imbalances, get enough rest, and keep all the love in your life.
Ask your doctor about taking high-dose vitamin D as needed to achieve a level of at least over 50 ng/ml. Which gets us back to #1... know your blood vitamin D level.
Knowing My Vitamin D Replacement
To know how much vitamin D to take, you either A) know your blood level, or B) you don’t.
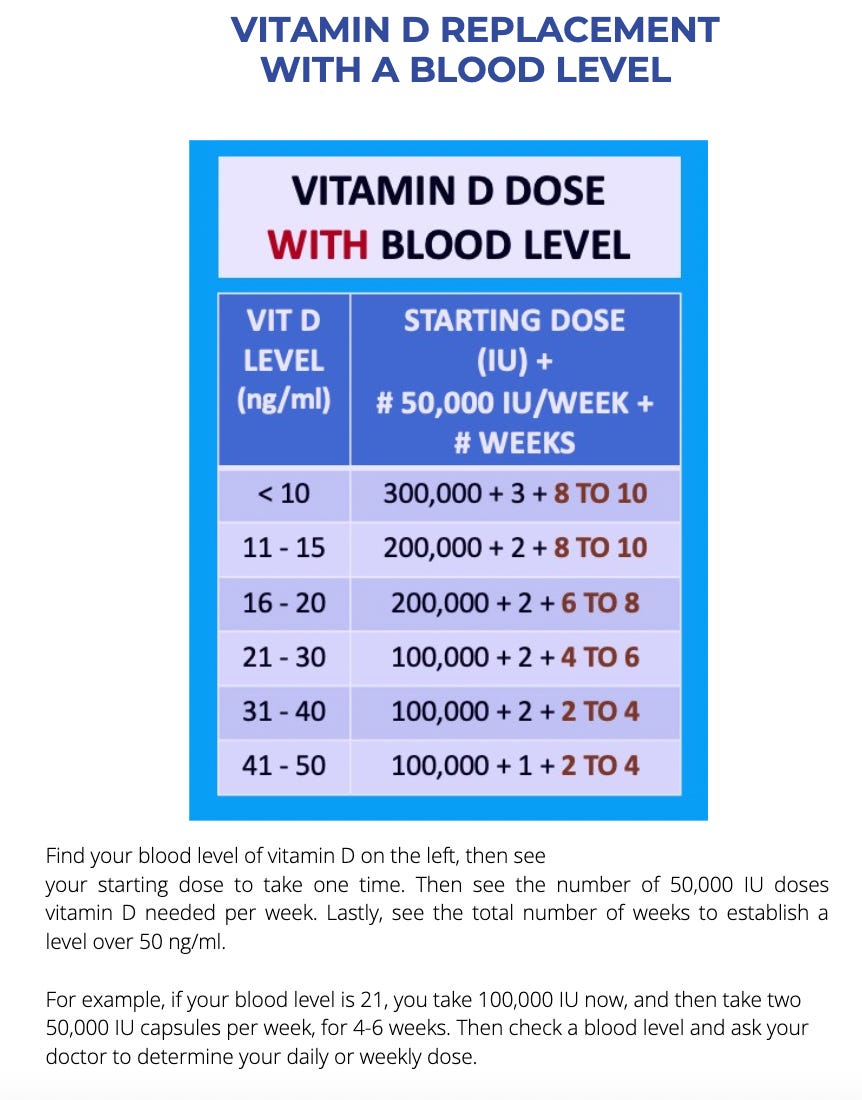
A. When You Know Your Vitamin D Level
If you know your blood vitamin D level, simply look at the chart to see how much vitamin D3 you should be taking:
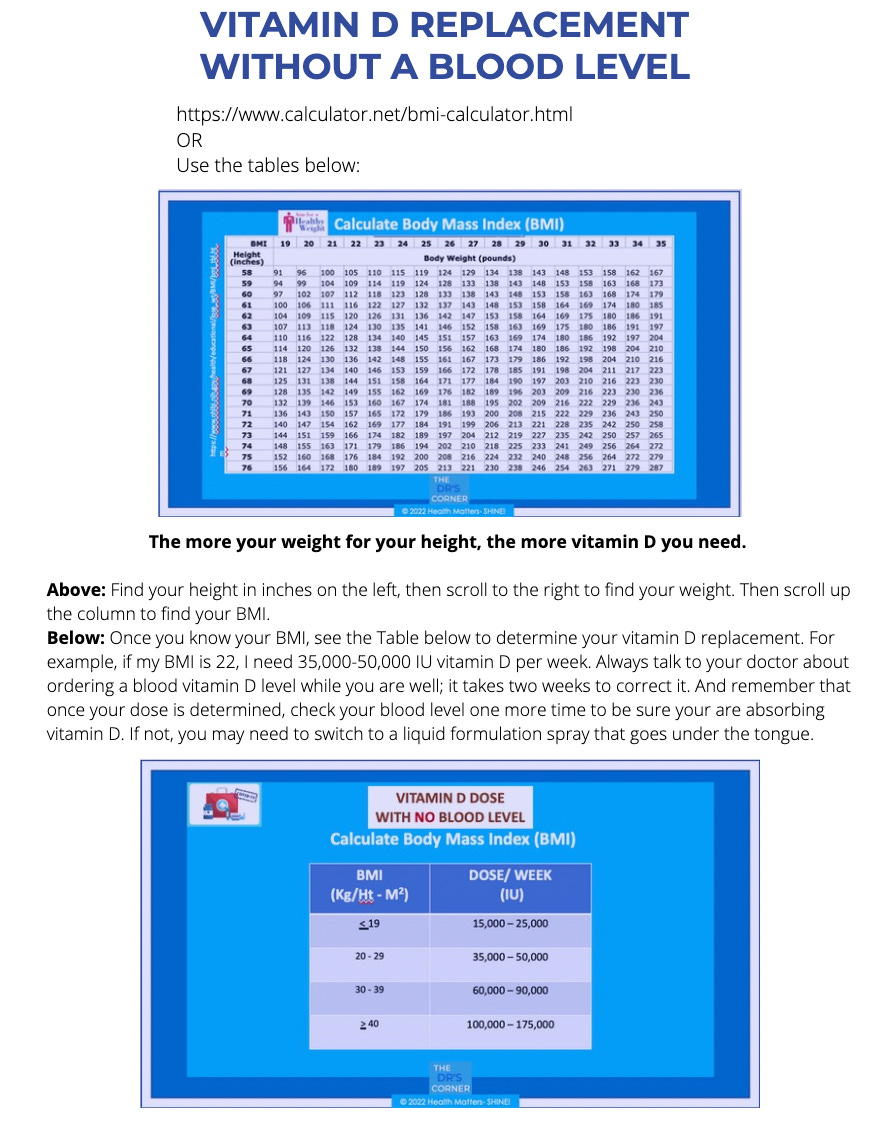
B. When You Don’t Know Your Vitamin D Level: Determine Your BMI First
Find your height on the top table, left side (y axis). If you are 5 feet tall, that is 60 inches (5 x 12).
Find your weight on row to its right. If I weigh 128 lb, my BMI is 25.
Once your BMI is known, replace vitamin D with the chart. If my BMI is 25, I am in group that is 20-29. My replacement is 35,000 to 50,000 IU per week.
I have 3 Options:
A. Take one 5,000 IU capsule vitamin D a day = 35,000 IU/week.
B. I can take 2 on the weekends, = (5,000 x 5 days = 25,000) + (10,000 x 2 days = 20,000) = 45,000 IU.
I could even double my dose 3 days/week, = (5,000 x 4 days = 20,000) + (10,000 x 3 days = 30,000) = 50,000.
I hope you find this useful, and that it makes sense. If you have trouble or want a confirmation on your math, just leave a comment below and we’ll help you out.
What Kind of Vitamin D Should I Take?
Vitamin D3 + vitamin K2 keeps calcium in the bones, instead of the arteries. Together, each increases the absorption of the other.
I like Metagenics because they're physician-grade formulas.
You may as well get everything in one package:
Here’s my best recommendation on a vitamin D3 + K2 formulation:
And if you've been suffering from chronic pain or fatigue, maybe your adrenal glands need a boost:
Can’t sleep? https://margaretaranda.metagenics.com/benesom
Because The Rebel Patient knows who she is. The Rebel Patient reads and understands more than he gets credit for, and isn’t afraid to speak up. Like a rebel, she is always thinking and if needed, she is willing to defend herself. He knows his body. He will search until he has a diagnosis, and keep trying different things before giving up. Then he seeks the best available treatment.
Most of all, rebel patients are growing in number and choosing the specialists that still uphold the Hippocratic Oath: to do no harm ~ which means they have never told a patient to stay home until their lips turn blue. And they never will.
MEDICAL DISCLAIMER: Nothing in this article is meant for personal medical advice nor replaces a personal assessment and evaluation by a qualified medical professional. Seek medical care if you are not feeling well. Never take anything on the internet as something you as an individual should specifically do. Material is for general and educational purposes. None of these comments have been evaluated by the FDA and no diseases are cured by vitamin D.
References
1. Review. Immunologic Effects of Vitamin D on Human Health and Disease. Charoenngam N, Holick MFNutrients. 2020 Jul 15; 12(7). [PubMed] [Ref list]
2. Review. Vitamin D deficiency as a risk factor for infection, sepsis and mortality in the critically ill: systematic review and meta-analysis. de Haan K, Groeneveld AB, de Geus HR, Egal M, Struijs ACrit Care. 2014 Dec 5; 18(6):660. [PubMed] [Ref list]
3. Association of low serum 25-hydroxyvitamin D levels and mortality in the critically ill. Braun A, Chang D, Mahadevappa K, Gibbons FK, Liu Y, Giovannucci E, Christopher KBCrit Care Med. 2011 Apr; 39(4):671-7. [PubMed] [Ref list]
4. Vitamin D supplementation to prevent acute respiratory infections: individual participant data meta-analysis. Martineau AR, Jolliffe DA, Greenberg L, Aloia JF, Bergman P, Dubnov-Raz G, Esposito S, Ganmaa D, Ginde AA, Goodall EC, Grant CC, Janssens W, Jensen ME, Kerley CP, Laaksi I, Manaseki-Holland S, Mauger D, Murdoch DR, Neale R, Rees JR, Simpson S, Stelmach I, Trilok Kumar G, Urashima M, Camargo CA, Griffiths CJ, Hooper RLHealth Technol Assess. 2019 Jan; 23(2):1-44. [PubMed] [Ref list]
5. Vitamin D supplementation to prevent acute respiratory infections: individual participant data meta-analysis. Martineau AR, Jolliffe DA, Greenberg L, Aloia JF, Bergman P, Dubnov-Raz G, Esposito S, Ganmaa D, Ginde AA, Goodall EC, Grant CC, Janssens W, Jensen ME, Kerley CP, Laaksi I, Manaseki-Holland S, Mauger D, Murdoch DR, Neale R, Rees JR, Simpson S, Stelmach I, Trilok Kumar G, Urashima M, Camargo CA, Griffiths CJ, Hooper RLHealth Technol Assess. 2019 Jan; 23(2):1-44. [PubMed] [Ref list]
6. Review. Regulation of Immune Function by Vitamin D and Its Use in Diseases of Immunity. Vanherwegen AS, Gysemans C, Mathieu C. Endocrinol Metab Clin North Am. 2017 Dec; 46(4):1061-1094. [PubMed] [Ref list]
7. Review. Modulation of the immune response to respiratory viruses by vitamin D. Greiller CL, Martineau ARNutrients. 2015 May 29; 7(6):4240-70. [PubMed] [Ref list]
8. Serum 25-hydroxyvitamin d and the incidence of acute viral respiratory tract infections in healthy adults. Sabetta JR, DePetrillo P, Cipriani RJ, Smardin J, Burns LA, Landry ML.PLoS One. 2010 Jun 14; 5(6):e11088. [PubMed] [Ref list]
9. Association of vitamin D deficiency with severity of acute respiratory infection: A case-control study in New Zealand children. Ingham T.R., Jones B., Camargo C.A., Kirman J., Dowell A.C., Crane J. Eur Respir. J. Eur. Respir. Soc. 2014;44:124. [Google Scholar] [Ref list]
10. Review. The role of vitamin D in prevention and treatment of infection. Gunville CF, Mourani PM, Ginde AA. Inflamm Allergy Drug Targets. 2013 Aug; 12(4):239-45. [PubMed] [Ref list]
11. Review. Translating the role of vitamin D3 in infectious diseases.Khoo AL, Chai L, Koenen H, Joosten I, Netea M, van der Ven A. Crit Rev Microbiol. 2012 May; 38(2):122-35.
12. Review. The Relationship Between Vitamin D and Infections Including COVID-19: Any Hopes? Taha R, Abureesh S, Alghamdi S, Hassan RY, Cheikh MM, Bagabir RA, Almoallim H, Abdulkhaliq A. Int J Gen Med. 2021; 14():3849-3870. [PubMed] [Ref list]
13. Review Vitamin D supplementation to prevent acute respiratory tract infections: systematic review and meta-analysis of individual participant data. Martineau AR, Jolliffe DA, Hooper RL, Greenberg L, Aloia JF, Bergman P, Dubnov-Raz G, Esposito S, Ganmaa D, Ginde AA, Goodall EC, Grant CC, Griffiths CJ, Janssens W, Laaksi I, Manaseki-Holland S, Mauger D, Murdoch DR, Neale R, Rees JR, Simpson S Jr, Stelmach I, Kumar GT, Urashima M, Camargo CA Jr. BMJ. 2017 Feb 15; 356():i6583. [PubMed] [Ref list]
14. Vitamin D deficiency contributes directly to the acute respiratory distress syndrome (ARDS). Dancer RC, Parekh D, Lax S, D'Souza V, Zheng S, Bassford CR, Park D, Bartis DG, Mahida R, Turner AM, Sapey E, Wei W, Naidu B, Stewart PM, Fraser WD, Christopher KB, Cooper MS, Gao F, Sansom DM, Martineau AR, Perkins GD, Thickett DR. Thorax. 2015 Jul; 70(7):617-24. [PubMed] [Ref list]
15. Association between prehospital vitamin D status and incident acute respiratory failure in critically ill patients: a retrospective cohort study.Thickett DR, Moromizato T, Litonjua AA, Amrein K, Quraishi SA, Lee-Sarwar KA, Mogensen KM, Purtle SW, Gibbons FK, Camargo CA Jr, Giovannucci E, Christopher KB. BMJ Open Respir Res. 2015; 2(1):e000074.
16. COVID-19 Mortality Risk Correlates Inversely with Vitamin D3 Status, and a Mortality Rate Close to Zero Could Theoretically Be Achieved at 50 ng/mL 25(OH)D3: Results of a Systematic Review and Meta-Analysis. Lorenz Borsche, Bernd Glauner, and Julian von Mendel. Nutrients. 2021 Oct; 13(10): 3596.
Thank you for keeping in prayer for Karen Kingston and her family. God bless you in all that you do.
WHAT I REALLY THINK
Does your doctor know this stuff?
Keep reading with a 7-day free trial
Subscribe to The Rebel Patient™ to keep reading this post and get 7 days of free access to the full post archives.