"Booster Brain": New Onset Psychosis and Brain White Matter Abnormalities from the Covid Jab
Within 7 Days of Getting the Jab
The Tweet
Source: https://x.com/harryfisheremtp/status/1857517087544979689?s=46
The Video
Abnormalities after the injection include a immune response, autoimmune disease, in the brain include stress, anxiety, and FLAIR, FLuid-Attenuated Abnormalities In the bRain, and hyperintensities in the white matter:
The Thread
Update on CDC Covid Vax Side Effects
Explanation: Judith says this vax “side effect” “rule” is that a psychosis occured within the first 5 days - but the rule says it “doesn't count” unless it occurs after 14 days.
If you look at the CD website, it says you can sign up for the V-safe website and they'll text you questions pertaining to side effects, with the first text occurring at one week, and thereafter for six weeks total:
Source: https://www.cdc.gov/vaccine-safety-systems/v-safe/faqs.html
And the CDC website says you can report side effects if you got them in the last 42 days (for anyone 6 months and older):
Source: https://www.cdc.gov/vaccine-safety-systems/v-safe/index.html
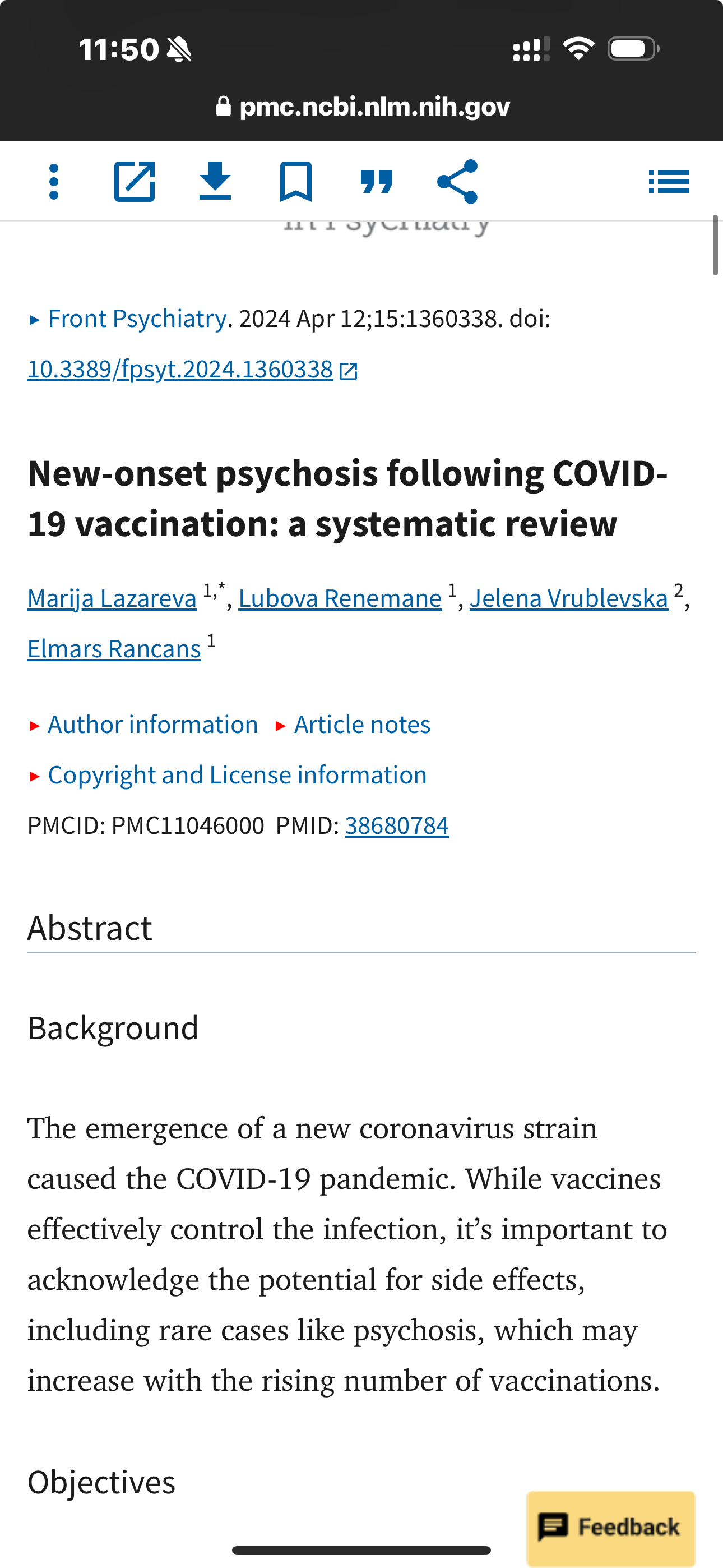
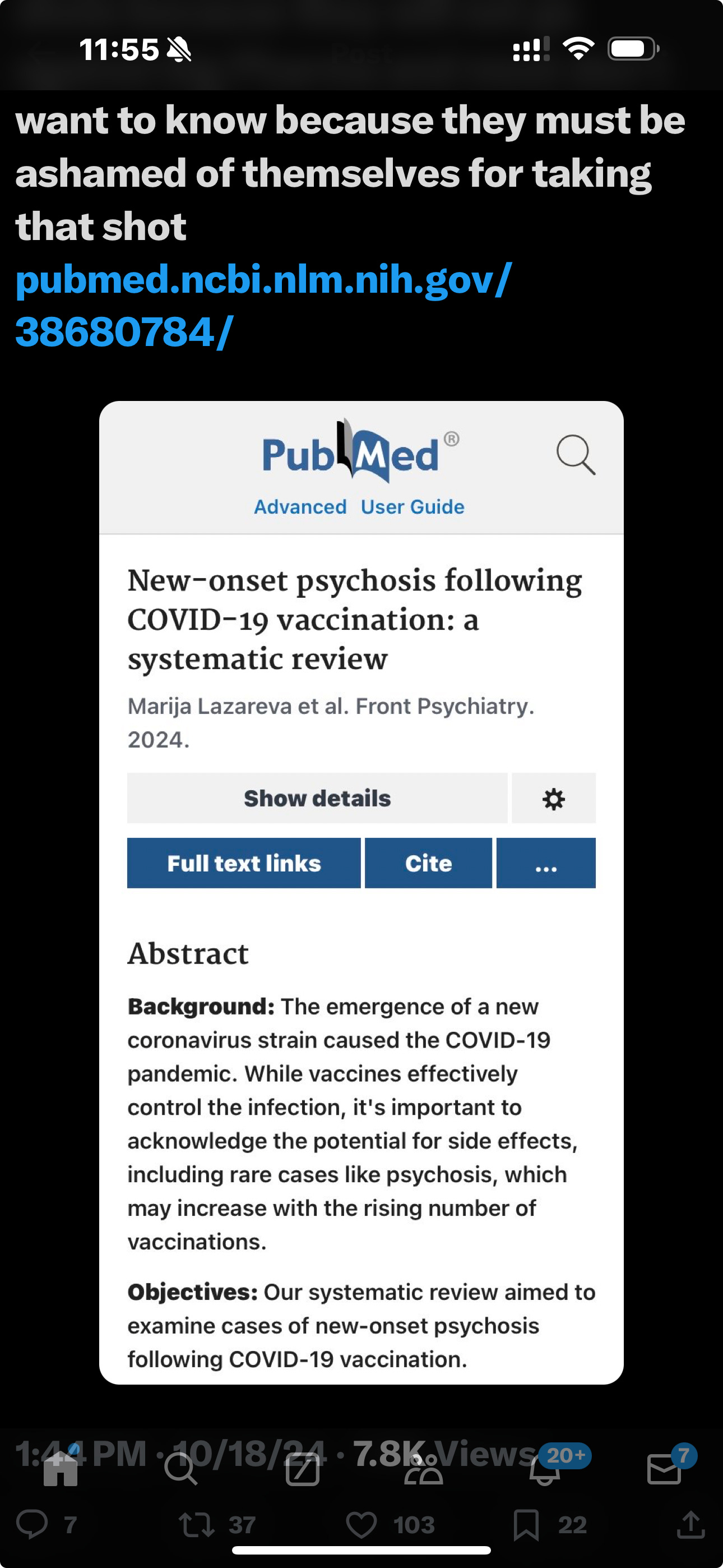
Abstract
Background
The emergence of a new coronavirus strain caused the COVID-19 pandemic. While vaccines effectively control the infection, it’s important to acknowledge the potential for side effects, including rare cases like psychosis, which may increase with the rising number of vaccinations.
Objectives
Our systematic review aimed to examine cases of new-onset psychosis following COVID-19 vaccination.
Methods
We conducted a systematic review of case reports and case series on new-onset psychosis following COVID-19 vaccination from December 1st, 2019, to November 21st, 2023, using PubMed, MEDLINE, ClinicalKey, and ScienceDirect. Data extraction covered study and participant characteristics, comorbidities, COVID-19 vaccine details, and clinical features. The Joanna Briggs Institute quality assessment tools were employed for included studies, revealing no significant publication bias.
Results
A total of 21 articles described 24 cases of new-onset psychotic symptoms following COVID-19 vaccination. Of these cases, 54.2% were female, with a mean age of 33.71 ± 12.02 years. Psychiatric events were potentially induced by the mRNA BNT162b2 vaccine in 33.3% of cases, and psychotic symptoms appeared in 25% following the viral vector ChAdOx1 nCoV-19 vaccine. The mean onset time was 5.75 ± 8.14 days, mostly reported after the first or second dose. The duration of psychotic symptoms ranged between 1 and 2 months with a mean of 52.48 ± 60.07 days. Blood test abnormalities were noted in 50% of cases, mainly mild to moderate leukocytosis and elevated C-reactive protein. Magnetic resonance imaging results were abnormal in 20.8%, often showing fluid-attenuated inversion recovery hyperintensity in the white matter. Treatment included atypical antipsychotics in 83.3% of cases, typical antipsychotics in 37.5%, benzodiazepines in 50%, 20.8% received steroids, and 25% were prescribed antiepileptic medications. Overall, 50% of patients achieved full recovery.
Conclusion
Studies on psychiatric side effects post-COVID-19 vaccination are limited, and making conclusions on vaccine advantages or disadvantages is challenging. Vaccination is generally safe, but data suggest a potential link between young age, mRNA, and viral vector vaccines with new-onset psychosis within 7 days post-vaccination. Collecting data on vaccine-related psychiatric effects is crucial for prevention, and an algorithm for monitoring and treating mental health reactions post-vaccination is necessary for comprehensive management.
Systematic review registration
https://www.crd.york.ac.uk/PROSPERO, identifier CRD42023446270.
Keywords: SARS-CoV-2, COVID-19, vaccination, new-onset psychosis, adverse effects
Source: https://pmc.ncbi.nlm.nih.gov/articles/PMC11046000/
The above paper describes a range of abnormalities discussed above. Here is the MRI-related information:
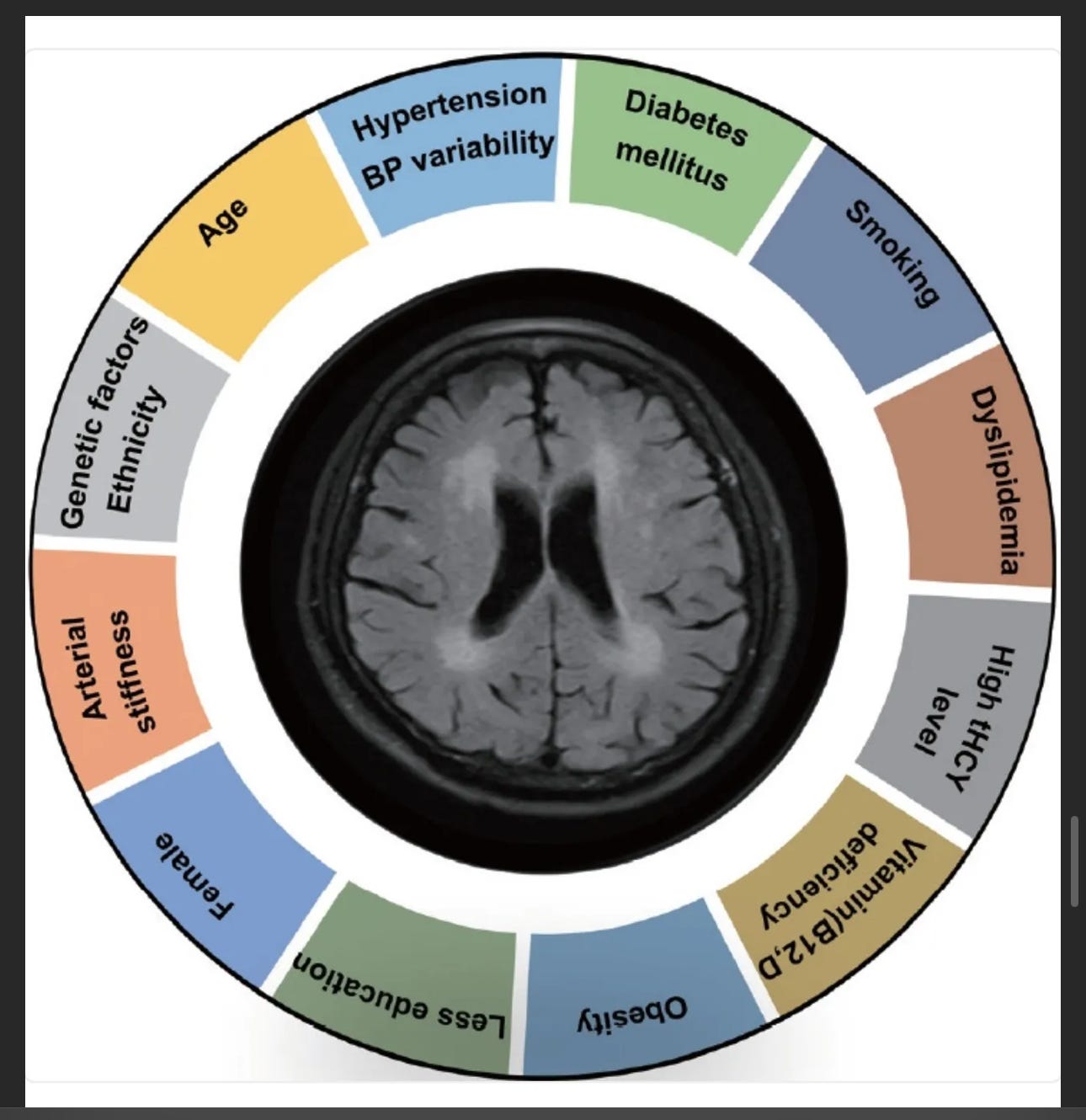
Leukoaraiosis
“Leuko” means “white”, e.g. leukocytes, as in white blood cells that fight infection. The white matter of the brain is the two large curly hemispheres filled with nerve cells. “Araiosis” means “rarefaction”. It was originally described in 1986 by Hachinski and colleagues [Ref 3] to describe hypodense cerebral white matter abnormalities on CT scans or hyperintensities on T2-weighted magnetic resonance imaging (MRI) scans [Ref 1-3].
Leukoaraiosis is also known as white matter hyperintensities (WMHs) or white matter lesions (WMLs).
Abstract
Leukoaraiosis (LA) manifests as cerebral white matter hyperintensities on T2-weighted magnetic resonance imaging scans and corresponds to white matter lesions or abnormalities in brain tissue. Clinically, it is generally detected in the early 40s and is highly prevalent globally in individuals aged >60 years. From the imaging perspective, LA can present as several heterogeneous forms, including punctate and patchy lesions in deep or subcortical white matter; lesions with periventricular caps, a pencil-thin lining, and smooth halo; as well as irregular lesions, which are not always benign. Given its potential of having deleterious effects on normal brain function and the resulting increase in public health burden, considerable effort has been focused on investigating the associations between various risk factors and LA risk, and developing its associated clinical interventions. However, study results have been inconsistent, most likely due to potential differences in study designs, neuroimaging methods, and sample sizes as well as the inherent neuroimaging heterogeneity and multi-factorial nature of LA. In this article, we provided an overview of LA and summarized the current knowledge regarding its epidemiology, neuroimaging classification, pathological characteristics, risk factors, and potential intervention strategies.
Keywords: Leukoaraiosis, White matter hyperintensities, White matter lesions, Imaging, Risk factors, Genetic variants.
…
LA generally manifests early in the fourth decade of life and becomes increasingly more common from age 50 onwards [4-6]. It is also common in healthy elderly individuals [4,7], and most individuals with LA remain asymptomatic. However, LA does not always represent benign imaging features, and could affect normal cognitive ability, motor function, and psychiatric behaviors if the WMLs expand to certain significant regions of the brain [8-13]. Clinically, LA has consistently been reported to be the most common radiological hallmark of cerebral small-vessel diseases (CSVDs) and as being strongly correlated with increased risks of cognitive function decline [14-17], motor gait dysfunction [10,18-20], stroke [21-26], dementia [16,17,21,25], depression [27-30], and even death [21,25,26], Given the clinical importance of WMHs in geriatric populations, there is an urgent need to understand the clinical features and pathogenesis of LA and develop effective strategies for its prevention and management.
…
Epidemiology of LA
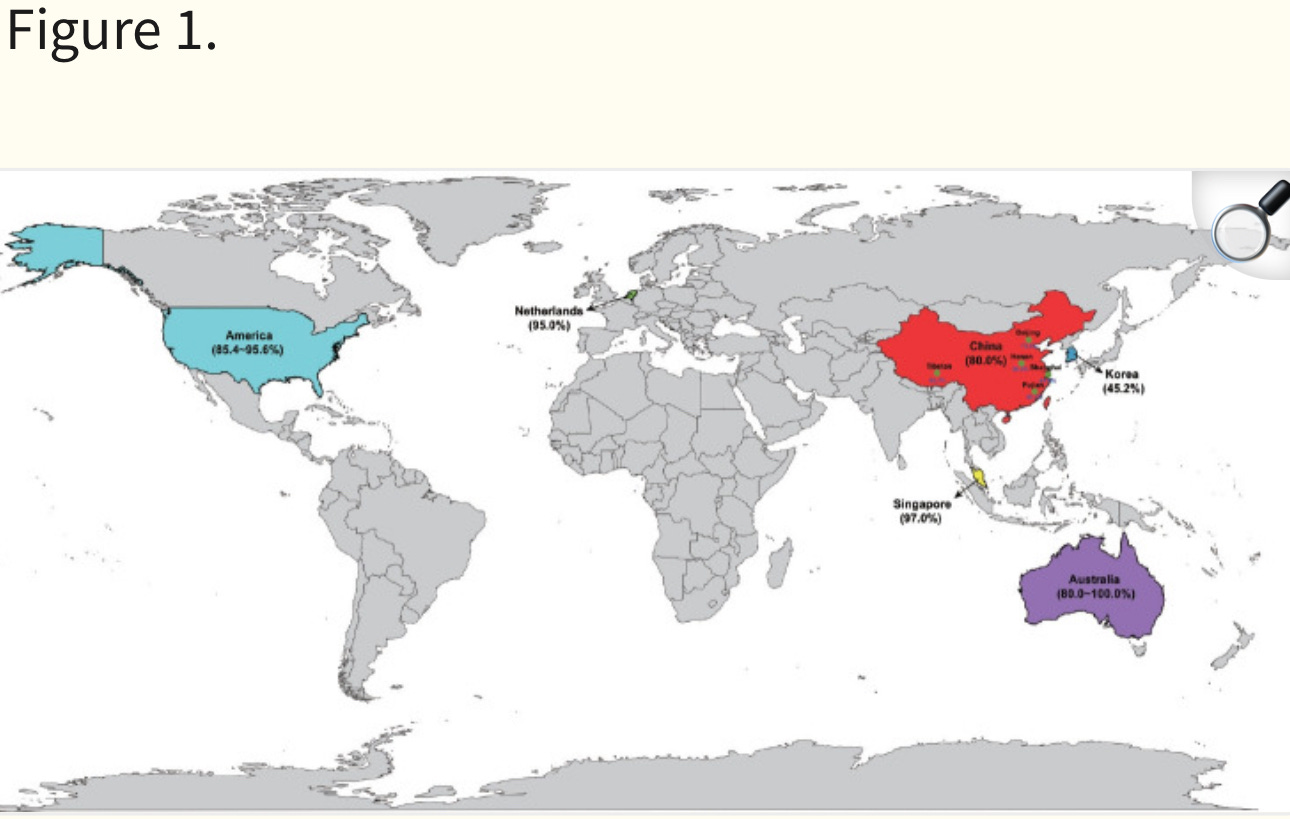
LA has a high prevalence globally among middle-aged and elderly individuals (36.5%–100% over age 40 years) [4,31-37]. Based on community-based studies in Australia and European countries (including Italy, Spain, France, Netherlands, UK, Sweden, Austria, Germany, and Poland), the incidence of LA in the general population can be as high as 80.0% and 92%, respectively [31,32]. Population-based studies in the Netherlands and Australia have also revealed a high prevalence (up to 95% and 100% in individuals aged >60 years, respectively) [33,34]. Similarly, the incidence of LA in the community-based population in the USA is also high, with the Cardiovascular Health Study and Atherosclerosis Risk in Communities Study reporting an incidence of 85.4%–95.6% in participants aged >55 years (Figure 1) [4,35]; moreover, its reported prevalence is higher among European-Americans (90.2%) than among African-Americans (80.6%) [35]. Recently, the largest community-based study in Asian cities (including Hong Kong, Singapore, and Seoul) reported the prevalence of LA as being up to 85.6% among healthy subjects aged 60–89 years [36] (45.2% in Korea, 80.0% in China, and 97.0% in Singapore) [36] (Figure 1).
If you know someone who might have had brain changes after the jab, this is how you get the diagnosis:
FLAIR Imaging
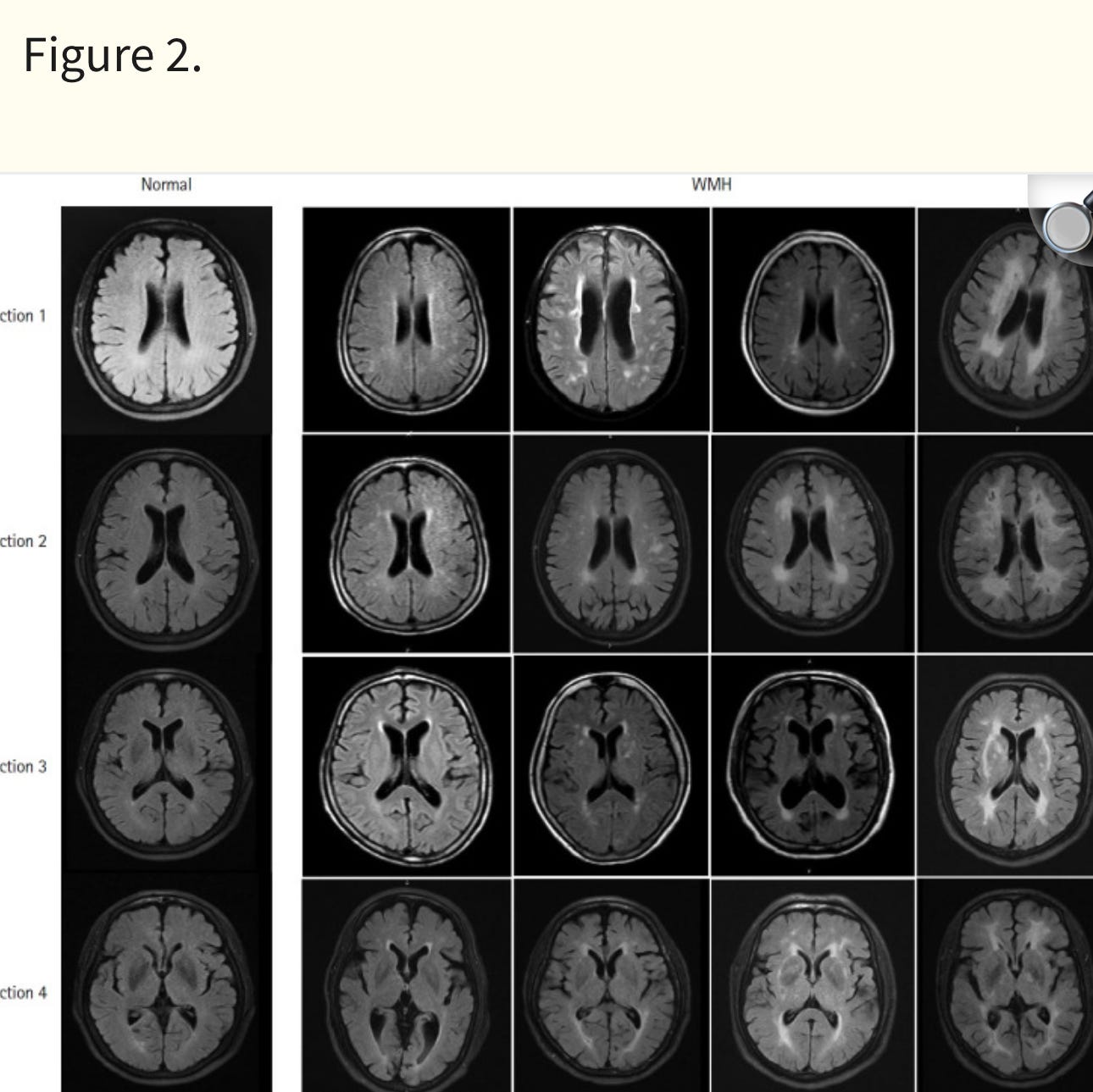
Fluid-attenuated inversion recovery (FLAIR) imaging is a form of heavily T2-weighted MRI with the advantage of cerebrospinal fluid (CSF) signal suppression (Figure 2) [44].
Compared to T2-weighted MRI, which simultaneously enhances WML and CSF signals and represents both as hyperintensities [45], FLAIR-MRI can efficiently differentiate WMLs from enlarged perivascular spaces that contain CSF (e.g., Virchow-Robin spaces), as they appear as hypointense regions on FLAIR-MRI. Thus, it greatly improves the detection efficiency of lesions adjacent to CSF-containing spaces and clearly distinguishes small periventricular WMLs (PVWMLs) from the ventricles [45-48]. Currently, FLAIR-MRI probably represents the best imaging method for assessing LA severity.
Several other advanced imaging methods are used for assessing white matter changes [2,48,49]. For example, diffusion tensor imaging (DTI) can not only assess the extent of white matter damage, but also provide information about the integrity of white matter tracts through apparent diffusion coefficient (ADC) or fractional anisotropy (FA) measurements of tissues, which reflect the directionality and rate of water mobility [50,51]. Altered microstructures both within WMLs and in normal-appearing white matter can be identified as regions of elevated ADC and decreased FA on DTI scans [52]. Therefore, DTI can be used to track early white matter changes over time and can provide insights into the in vivo pathogenesis of LA. T2-weighted gradient-recalled echo sequences and corresponding alternative-susceptibility weighted sequences with higher signal and spatial resolution are sensitive to iron deposition [53,54] and can therefore distinguish cerebral microbleeds as small round or ovoid hypointense lesions, which are features of hypertensive CSVD (such as cerebral amyloid angiopathy) as yet undetectable using conventional MRI [55,56].
There is a lot more detail on getting the diagnosis, and their summarizes the main variables and clinical presentations:
Risk Factors
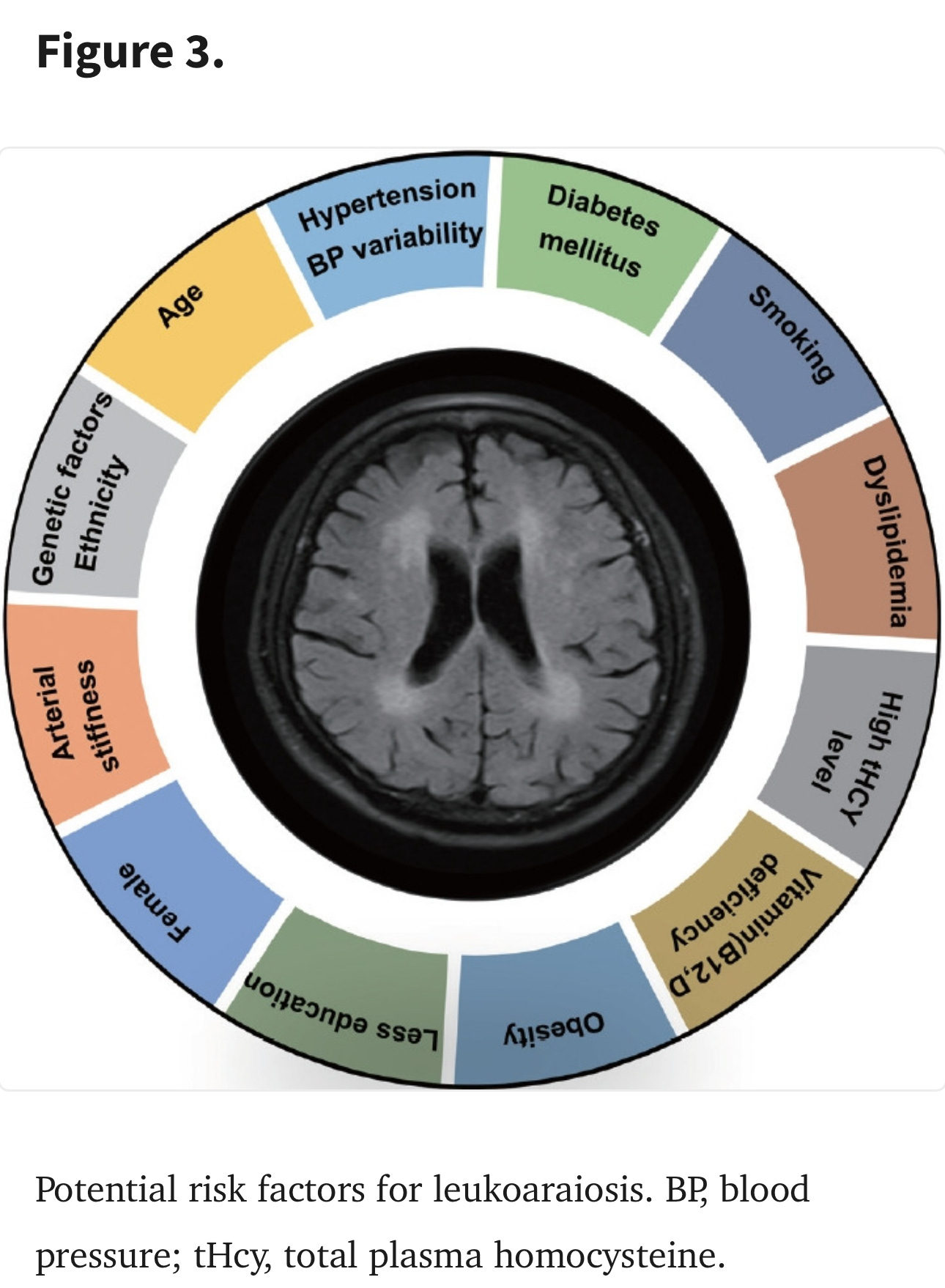
This section is also worth the read if it concerns you. The authors review each risk factor, with older age being the most important.
Management of LA
The imaging changes in LA are irreversible, as they eventually progress and enlarge to affect the surrounding cerebral white matter. Since the pathogenic mechanisms of LA are poorly understood, it is difficult to treat WMLs and reverse their formation. Therefore, what matters most currently is to delay the onset of LA, attenuate its progression, and reduce its incidence and severity through effective strategies. To our knowledge, the current prevention and management methods for LA are mostly empirical and mainly target vascular risk factors to prevent or delay the progression of LA through pharmacological interventions. During the past twenty years, more and more evidence has shown the efficiency of controlling for vascular risk factors in the management of LA. Here, we have reviewed these potential intervention strategies.
Conclusion and Perspectives
Although we have known about the concept of LA for about three decades, its significance in the clinical and academic fields is somewhat underestimated by physicians and neurologists compared to those age-related neurodegenerative conditions such as Parkinson’s disease, Alzheimer’s disease, and stroke. With improvements in imaging technologies and the widespread use of FLAIR-MRI in community hospitals, as well as the increased rate of aging in society, more and more cases of LA are being encountered. This has also led to an increased public awareness about LA.
This review article provides an overview of the current advances related to LA for professionals as well as the general public. A better understanding of the imaging heterogeneity, histopathological characteristics, and clinical risk factors of LA will greatly promote our understanding of its nature. The significant associations between certain risk factors (such as age, hypertension, elevated homocysteine level, arterial stiffness) with LA incidence not only offer specific clues regarding its pathogenesis, but also suggest potential intervention strategies for its management. In view of the consistently positive results from clinical association studies and prospective RCTs, controlling key cardiovascular risk factors (such as BP, blood lipid levels) and maintaining a healthy lifestyle (by smoking cessation, physical exercise, healthy diet) should be efficient strategies for preventing the onset and progression of LA.
Additionally, although the heterogeneous histopathological and imaging characteristics of WMHs provide key clues regarding etiology, the underlying molecular mechanisms in LA remain unclear. Genetic studies (especially GWASs) have identified some susceptibility genes for LA and its subclasses in the past decade, which also offer many possibilities for exploring its pathogenesis. Genomic and molecular pathological mechanisms specific to LA subtypes may also represent promising research avenues in the future. Similarly, the identification of biological processes and signaling pathways specific to LA subtypes or its onset and development will help to clarify its pathogenesis and provide potential drug targets and intervention strategies for treatment. This is critical for reducing the public health burden and will benefit aging societies all around the world. Thus, further efforts are needed to construct comprehensive LA models and conduct genetic studies on LA in animals in parallel with clinical studies.
Source: https://pmc.ncbi.nlm.nih.gov/articles/PMC11164597/
I hope this article helps to bring some light on the brain issues associated with the jab. But I didn't just want to leave it with that alone.
This is an excellent paper that further describes the imaging studies that can surface after the jab, or with aging and other risk factors. While no definitive treatment is known, rest assured that God is bigger than anything and He can 💯 % heal you from any beain injury.
How do I know this as a fact? Because I am a living example.







I bet SSRI, SNRI and anti psychotic sales are booming 🤦🏻♀️😞🤮